How Sauna Helps Chronic Inflammation: Science, Protocol & Safety
Regular sauna use is associated with lower levels of systemic inflammatory markers like high-sensitivity C-reactive protein (hsCRP) and may support better cardiovascular outcomes, though most evidence comes from observational studies rather than randomized trials.
Key takeaways:
- Finnish men using saunas 4–7 times per week had significantly lower hsCRP (1.65 mg/L) compared to once-weekly users (2.41 mg/L), a difference of −0.84 mg/L.
- Acute sauna sessions increase certain cytokines like IL-6 and IL-1RA without immediately lowering CRP; benefits appear with frequent long-term use.
- Traditional Finnish saunas have the strongest evidence for systemic inflammation and mortality reduction; infrared saunas show promise for symptom relief in chronic pain conditions.
- Sessions of 10–20 minutes, 2–4 times per week (or more for experienced users), appear safe for most healthy adults when proper hydration and safety precautions are followed.
- Critical caution: Sauna is contraindicated during acute illness, hypertensive crisis, unstable angina, recent heart attack, or severe aortic stenosis.
Table of Contents
- What Is Chronic Inflammation—and Why It Matters
- The Core Mechanism—How Heat Therapy Affects Inflammation
- Key Inflammatory Markers—CRP and Beyond
- Infrared vs Traditional—Which Sauna for Inflammation?
- Acute vs Chronic—When to Use Sauna and When to Avoid It
- The Optimal Sauna Protocol for Chronic Inflammation
- Decision Tree—Match Your Condition to Your Sauna
- Safety, Contraindications, and Hydration
- Secondary Benefits—Pain Relief, Circulation, Longevity
- Frequently Asked Questions
- Sources
- What We Still Don't Know
What Is Chronic Inflammation—and Why It Matters
Chronic inflammation is a persistent, low-grade activation of the immune system that lasts for months or years, distinct from the short-lived acute inflammation that follows injury or infection. While acute inflammation helps you heal, chronic inflammation operates quietly in the background, contributing to higher risks of cardiovascular disease, type 2 diabetes, and all-cause mortality (PubMed, 2018).
The marker most studied in sauna research is high-sensitivity C-reactive protein (hsCRP), a liver-produced protein that rises in response to systemic inflammation. Elevated hsCRP correlates with increased risk of heart attack, stroke, and death from cardiovascular causes. In a prospective Finnish cohort of 2,084 men followed for 11 years, those using saunas 4–7 times per week had mean hsCRP of 1.65 mg/L compared to 2.41 mg/L in men using saunas once per week—a statistically significant difference of −0.84 mg/L (PubMed, 2018).
A related study of 2,575 Finnish men found that both high hsCRP and infrequent sauna use independently predicted higher mortality. Importantly, frequent sauna bathing appeared to offset the increased mortality risk associated with elevated hsCRP, suggesting an interaction between inflammation level and sauna exposure (PMC, 2022).
Critical context: These studies are observational, not randomized controlled trials. They cannot prove that sauna use alone causes lower inflammation or longer life. Men who use saunas frequently may also exercise more, eat better, and engage in other healthy behaviors. Sauna should be viewed as a supportive lifestyle tool—not a cure or disease-modifying therapy for autoimmune or inflammatory conditions.
<a name="core-mechanism"></a>
The Core Mechanism—How Heat Therapy Affects Inflammation
Sauna bathing induces controlled heat stress that activates multiple physiological responses: increased heart rate, widespread vasodilation, profuse sweating, and activation of molecular stress pathways.
Heat shock proteins (HSPs) are key mediators in this process. When your body experiences heat stress, production of certain HSPs increases. These protective molecules assist protein folding, protect cells from damage, and can modulate inflammatory signaling. A 4-week hot-water immersion study in fibromyalgia patients showed that heat therapy reduced HSP90 while increasing HSP40 and HSC70, alongside improvements in pain and physical function—without significant changes in measured pro- or anti-inflammatory markers (PMC, 2025).
Acute vs Chronic Inflammatory Response to Heat
Here's where sauna's effects on inflammation become nuanced: acute sauna sessions actually increase some inflammatory mediators, while frequent long-term use is associated with lower baseline inflammatory markers.
A crossover study of Finnish sauna bathing in healthy middle-aged and older adults found that two 10-minute sessions significantly increased interleukin-6 (IL-6) and IL-1 receptor antagonist (IL-1RA), while CRP did not change acutely (ScienceDirect, 2020). This might sound counterintuitive, but IL-6 is context-dependent. During exercise and heat exposure, IL-6 can play an anti-inflammatory, metabolic-regulating role—different from the chronic IL-6 elevation seen in inflammatory diseases.
Over time, frequent sauna use appears to train cellular stress-response systems and may down-regulate chronic inflammation, even though single sessions transiently raise some cytokines. The longitudinal Finnish cohort showed lower hsCRP and reduced mortality in frequent users, suggesting a chronic anti-inflammatory effect despite acute cytokine spikes (PubMed, 2018).
Heat therapy may also improve endothelial function, blood flow, and autonomic nervous system balance, which can indirectly reduce systemic inflammatory burden (UCLA Health, 2023).
Key Inflammatory Markers—CRP and Beyond
C-reactive protein (CRP/hsCRP) is the most studied systemic marker in sauna research. Higher sauna frequency is consistently associated with lower hsCRP in observational Finnish cohorts. However, this is a long-term association pattern—acute sauna sessions do not lower CRP immediately.
In the 2,084-man prospective study, participants were divided by sauna frequency:
- Once per week: mean hsCRP 2.41 mg/L
- 2–3 times per week: mean hsCRP 2.00 mg/L
- 4–7 times per week: mean hsCRP 1.65 mg/L
The adjusted difference between the highest and lowest frequency groups was −0.84 mg/L (95% CI −1.55 to −0.14), statistically significant even after controlling for age, cardiovascular risk factors, and lifestyle variables (PubMed, 2018).
Sauna and other cytokines: Acute sauna sessions may influence cytokines such as IL-6 and IL-1RA, with both increasing after sessions. However, consistent long-term changes in pro- and anti-inflammatory cytokines like TNF-α, IL-10, and others are not well demonstrated. The fibromyalgia heat therapy trial altered HSP expression and improved symptoms without significant changes in inflammatory markers, illustrating that symptom relief can occur without clear biomarker shifts (PMC, 2025).
What Current Studies Do NOT Show Yet
Writers and marketers often extrapolate beyond the data:
- No robust evidence for TNF-α suppression specific to sauna use in humans
- Limited data on IL-10 or other anti-inflammatory cytokines with sauna protocols
- No randomized controlled trials proving sauna reduces disease progression in autoimmune conditions
- Most evidence focuses on surrogate markers (hsCRP, cytokines) rather than hard clinical outcomes like reduced flares or slower joint damage
Stress that reductions in hsCRP may reflect overall lifestyle patterns—sauna use correlates with other healthy behaviors—rather than sauna alone.
<a name="infrared-vs-traditional"></a>
Infrared vs Traditional—Which Sauna for Inflammation?
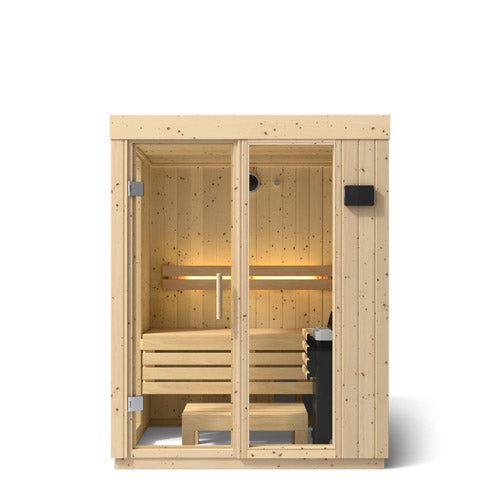
Traditional Finnish sauna uses high ambient temperature (typically 70–100°C) with heated stones and optional steam. Users sit or lie for 10–20 minutes, often in multiple bouts with cooling-down periods between.
Infrared sauna uses infrared emitters to heat the body directly at lower ambient temperatures (around 45–65°C). The infrared radiation penetrates skin and tissues, aiming to induce sweating and heat stress with potentially greater comfort for heat-sensitive individuals.
Evidence Strength by Sauna Type
Most long-term cohort data linking sauna to lower hsCRP, reduced cardiovascular events, and lower all-cause mortality come from traditional Finnish dry saunas, not infrared (PubMed, 2018; PMC, 2022; UCLA Health, 2023). These are observational studies in middle-aged and older Finnish men, so applicability to women, younger populations, and non-Finnish groups is uncertain.
Infrared sauna has much smaller, shorter trials focusing primarily on symptom relief and blood pressure. A review summarized in a hypertension article described infrared sauna research as showing "limited moderate evidence" for blood pressure normalization with no reported serious adverse effects (Healthgrades, 2021).
Evidence by Condition
Rheumatoid arthritis (RA) and ankylosing spondylitis (AS): A small clinical trial studied 17 RA patients and 17 AS patients who received 8 infrared sauna sessions over 4 weeks. Pain and stiffness decreased significantly during and after sessions (p < 0.05 in RA, p < 0.001 in AS), fatigue improved, and no exacerbation of disease activity scores was observed. However, improvements in disease activity over the 4 weeks did not reach statistical significance, and the trial was short with no control group (PubMed, 2009; University of Twente, 2017; The Polyclinic, 2022).
Fibromyalgia: A 12-week program combining traditional sauna and underwater exercise in 44 women led to 31–77% reductions in pain and symptom scores, maintained at 6-month follow-up. Separately, 4 weeks of hot-water immersion (not sauna, but similar heat therapy) reduced pain and improved physical function and sleep impairment (PubMed, 2011; PMC, 2025).
Practical differences relevant to inflammatory patients:
- Perceived comfort: Infrared's lower ambient temperature may be better tolerated by those who cannot handle high heat or have cardiovascular concerns.
- Heat intolerance: Individuals with low blood pressure or heat sensitivity often find infrared more comfortable (UCLA Health, 2023; Healthgrades, 2021).
- Equipment cost and installation: Infrared units are widely available as home models at various price points with smaller footprint; traditional saunas often require dedicated room installation.
- Evidence base: If your primary goal is systemic risk reduction and hsCRP-linked outcomes, traditional Finnish sauna has more robust evidence. For joint pain and stiffness in RA/AS, infrared sauna has some small clinical data for symptom relief.
Important caveat: Some patients report symptom worsening with infrared or heat. A Reddit user with ankylosing spondylitis described increased pain and flares after infrared sauna sessions, with their rheumatologist suggesting heat might exacerbate tendon-based inflammation (Reddit r/ankylosingspondylitis, 2025). This underscores individual variability—protocols should be personalized and adjusted if symptoms worsen.
Comparison Table: Traditional vs Infrared Sauna
| Dimension | Traditional Finnish Sauna | Infrared Sauna |
|---|---|---|
| Typical temperature | ~70–100°C ambient air | ~45–65°C ambient; infrared radiation heats body directly |
| Evidence for systemic inflammation (hsCRP) | Multiple Finnish cohorts link frequent use to lower hsCRP and reduced mortality | Limited; most data focus on blood pressure and symptom relief |
| Evidence for chronic inflammatory pain | Included in fibromyalgia thermal therapy; improved pain and quality of life | Small RA/AS trial shows short-term pain/stiffness relief without disease worsening |
| Tolerability for heat-sensitive users | Higher temperatures may be uncomfortable or poorly tolerated | Lower temperatures often better tolerated by those with heat intolerance or hypotension |
| Cardiovascular evidence base | Strongest; associated with lower CVD events and all-cause mortality | Limited; "limited moderate evidence" for blood pressure improvement, no major adverse effects |
| Practical considerations | Often requires dedicated room/installation; available in gyms/spas | Widely available as home units at various price points; smaller footprint |
| Suitability for autoimmune joint disease | No direct RA/AS RCTs, but heat can relieve stiffness in many patients | Some trial data for symptom relief; anecdotal reports of flares in spondyloarthritis with tendon involvement |
<a name="when-to-use-sauna"></a>
Acute vs Chronic—When to Use Sauna and When to Avoid It
Chronic systemic inflammation (persistent, low-grade immune activation) is different from acute inflammation (short-term response to injury, infection, or inflammatory flare). Understanding this distinction is critical for safe sauna use.
Sauna and heat therapy can be part of chronic inflammation management, but heat is generally not recommended during acute illness or uncontrolled inflammatory flares unless specifically cleared by a clinician.
When to Avoid Sauna
Cardiovascular contraindications (SIU School of Medicine, 2023):
- Unstable angina pectoris
- Recent myocardial infarction (heart attack)
- Severe aortic stenosis
Blood pressure concerns (Healthgrades, 2021):
- Hypertensive crisis (blood pressure ≥180/110 mmHg)—seek immediate medical help, do not use sauna
- Extremely low blood pressure without medical clearance
Other situations requiring caution:
- Acute illness or infection
- Acute joint flare in inflammatory arthritis
- Recent major surgery
- Pregnancy (consult physician)
- Dehydration or taking diuretic medications without medical guidance
Individual Variability in Autoimmune Conditions
While the RA/AS infrared sauna trial found no average disease exacerbation (PubMed, 2009), individual experiences vary. Heat can temporarily increase inflammation or pain in some people, particularly those with:
- Ankylosing spondylitis with significant tendon involvement
- Spondyloarthritis subtypes
- Active inflammatory flares
One patient with AS reported that infrared sauna triggered a perceived "surge in inflammation" and increased pain, especially affecting tendons and entheses (Reddit r/ankylosingspondylitis, 2025). Another user with RA noted initial discomfort but gradual tolerance with shorter, cooler sessions (Reddit r/rheumatoid, 2024).
Recommendation: If you have complex autoimmune disease, introduce sauna cautiously—start with short, lower-temperature sessions and monitor your response. Reduce time/temperature or discontinue if pain or disease activity consistently worsens.
<a name="optimal-protocol"></a>
The Optimal Sauna Protocol for Chronic Inflammation Relief
No single "anti-inflammatory sauna protocol" has been proven optimal in randomized trials. However, patterns emerge from the research:
Finnish sauna research protocols:
- Temperature: ~70–90°C
- Session length: 10–20 minutes per bout
- Structure: Often 2 bouts per session with cooling-down between
- Frequency: 2–4 times per week in trials; 4–7 times per week in cohorts with strongest outcomes (PubMed, 2018; PMC, 2022)
Infrared sauna protocols in clinical trials:
- Duration: ~15–20 minutes per session
- Frequency: 2 sessions per week in the 4-week RA/AS trial (PubMed, 2009)
Academic safety guidance for beginners and higher-risk individuals:
- Start with 5–10 minutes, gradually increasing to 15–20 minutes as tolerated (UCLA Health, 2023)
- Limit sessions to 10–15 minutes for people with heart disease or high blood pressure (Healthgrades, 2021)
- Hydrate generously before and after sessions
- Avoid alcohol before or during sauna (increases dehydration and arrhythmia risk)
- Monitor for dizziness, chest pain, or palpitations; exit immediately if these occur
Adapting Protocols for Age, Fitness Level, and Comorbidities
| User Profile | Session Duration | Frequency | Temperature Preference | Key Safety Notes |
|---|---|---|---|---|
| Healthy beginner, no major comorbidities | Start 5–10 minutes, gradually increase to 15–20 minutes | 2–3 times/week initially | Moderate (e.g., 70–80°C traditional or mid-range IR) | Hydrate before/after, avoid alcohol, exit if dizzy |
| Cardiometabolic risk (controlled hypertension, stable CVD) | 10–15 minutes per session | 2–4 times/week, depending on tolerance and physician input | Avoid extreme heat; favor moderate temperatures | Consult clinician; monitor for blood pressure changes, chest pain, or palpitations |
| Chronic pain/fibromyalgia | 10–20 minutes, possibly combined with low-impact exercise | 3 days/week sauna plus 2 days/week underwater exercise in one protocol | Select comfortable setting; may prefer gentle heat (IR or lower-temp traditional) | Introduce gradually; monitor fatigue and sleep; ensure hydration |
| Autoimmune arthritis (RA/AS) | ~15–20 minutes as tolerated; 8 sessions over 4 weeks used in IR trial | 2 sessions/week in 4-week IR trial | Lower-temperature IR often used in studies | Monitor for flares; stop if joints or tendons acutely worsen |
| Heat-sensitive/low blood pressure | Short sessions (5–10 minutes) | 1–3 times/week initially | Lower temperatures (IR or mild traditional) | Stand up slowly; ensure hydration; consider physician input |
Nuance: Evidence for an "optimal anti-inflammatory dose" is limited. Most data relate to cardiovascular outcomes and biomarkers rather than chronic pain or autoimmune disease endpoints. Personalization based on age, cardiovascular status, hydration, medication, and tolerance should shape your protocol.
<a name="decision-tree"></a>
Decision Tree—Match Your Condition to Your Sauna Type
Use this framework to navigate sauna selection based on your primary goal, heat tolerance, and underlying conditions:
If your primary goal is systemic risk reduction (lower hsCRP, cardiovascular protection): → Traditional Finnish sauna has the most evidence (PubMed, 2018; PMC, 2022; UCLA Health, 2023) → Frequency: 4–7 times/week in cohorts with strongest outcomes → Consider: Requires higher heat tolerance and often dedicated space or gym access
If your primary goal is chronic joint pain and stiffness relief (RA, AS, fibromyalgia): → Infrared sauna has small clinical data showing short-term symptom improvement (PubMed, 2009; University of Twente, 2017) → Traditional sauna included in fibromyalgia thermal therapy programs with positive results (PubMed, 2011) → Caution: Some spondyloarthritis patients report flares with infrared—monitor closely
If you have heat intolerance, low blood pressure, or cardiovascular concerns: → Infrared sauna at lower temperatures may be better tolerated (Healthgrades, 2021; UCLA Health, 2023) → Start with very short sessions (5–10 minutes) and build gradually → Consult your physician before beginning
If you're on a budget or have limited space: → Infrared home units are more accessible and compact → Traditional sauna access via gym membership or spa may be more cost-effective than home installation
If you prioritize the strongest research evidence base: → Traditional Finnish sauna for systemic inflammation, cardiovascular outcomes, and longevity → Acknowledge that infrared data are limited and mostly symptom-focused
Call-out: No head-to-head randomized controlled trials have compared infrared vs traditional sauna on chronic inflammatory markers or long-term outcomes. Both modalities can be part of a comprehensive inflammation management plan, but neither is a standalone cure.
Safety, Contraindications, and Hydration Protocols
Who should avoid sauna or seek medical clearance:
SIU School of Medicine identifies the following as conditions where sauna is not considered safe (SIU School of Medicine, 2023):
- Unstable angina pectoris
- Recent myocardial infarction
- Severe aortic stenosis
Healthgrades adds (Healthgrades, 2021):
- Hypertensive crisis (blood pressure >180/110 mmHg)—this is a medical emergency; seek immediate care
- Uncontrolled severe hypertension
- Acute illness or infection
UCLA Health recommends consultation for (UCLA Health, 2023):
- Pregnancy
- Very low blood pressure
- Significant cardiovascular disease
Hydration and Electrolyte Management
Critical safety practices:
- Drink water before and after sauna sessions to prevent dehydration
- Avoid alcohol before, during, or immediately after sauna—alcohol substantially increases risk of dehydration, hypotension, arrhythmias, and even death in extreme cases (SIU School of Medicine, 2023; Healthgrades, 2021; UCLA Health, 2023)
- If you take diuretic medications or sweat heavily, consider electrolyte replacement
- Weigh yourself before and after to gauge fluid loss; aim to replace lost fluids
Red Flags—When to Stop a Session and Seek Medical Care
Exit the sauna immediately and seek medical attention if you experience:
- Dizziness or lightheadedness (especially if severe or not resolving with cooling)
- Chest pain or pressure
- Palpitations or irregular heartbeat
- Severe shortness of breath
- Confusion or feeling faint
Nuance on overall safety: Sauna use appears relatively safe for healthy adults and even many people with stable cardiovascular disease when used appropriately. However, the margin of safety narrows with comorbidities and extreme heat exposures. Most safety data come from supervised environments like Finnish public saunas; home units may lack oversight, so extra caution is warranted (SIU School of Medicine, 2023; Healthgrades, 2021; UCLA Health, 2023).

Secondary Benefits—Pain Relief, Circulation, and Longevity
Chronic Pain and Quality of Life
Beyond systemic inflammatory markers, heat therapy and sauna show benefits for pain and function:
Fibromyalgia: A 12-week program combining sauna with underwater exercise in 44 women led to 31–77% reductions in pain and symptom scores using validated questionnaires like the Fibromyalgia Impact Questionnaire. Improvements were maintained at 28–68% at 6-month follow-up (PubMed, 2011). A separate 4-week hot-water immersion trial decreased average and worst pain scores and improved physical function and sleep impairment (PMC, 2025).
RA and AS: The infrared sauna trial showed improved pain and stiffness during and after sessions without worsening disease activity, though disease activity changes over 4 weeks were not statistically significant (PubMed, 2009; The Polyclinic, 2022).
Mechanism: These benefits likely involve increased blood flow, endothelial function improvements, HSP-mediated cellular protection, and neural pain modulation—not necessarily reductions in inflammatory cytokines. The fibromyalgia heat therapy study showed HSP changes and symptom improvements without significant pro- or anti-inflammatory marker shifts (PMC, 2025).
Cardiovascular Health and Longevity
Finnish cohort studies link frequent sauna use to:
- Reduced blood pressure
- Improved vascular health
- Lower risk of stroke
- Reduced fatal cardiovascular events
- Lower all-cause mortality
In one cohort, men using saunas 4–7 times per week had significantly lower cardiovascular and all-cause mortality compared to once-weekly users. The inflammation pathway (hsCRP) appears to be one mediating mechanism (PubMed, 2018; PMC, 2022; UCLA Health, 2023).
Critical context: Many of these benefits are symptom-level and quality-of-life improvements, not structural disease reversal. Interventions often occurred alongside other therapies (exercise, medications), so isolating sauna's unique contribution is difficult.
<a name="faqs"></a>
Frequently Asked Questions
1. Does using a sauna actually help reduce chronic inflammation?
Regular sauna use is associated with lower levels of hsCRP and may support lower systemic inflammation, but most evidence is observational rather than from randomized trials.
- Finnish men using saunas 4–7 times/week had significantly lower hsCRP than men using them once/week (PubMed, 2018).
- Frequent sauna bathing appeared to offset mortality risk associated with high hsCRP (PMC, 2022).
- Acute sessions raise some cytokines like IL-6 and IL-1RA without immediate CRP changes (ScienceDirect, 2020).
- Sauna should be viewed as an adjunct to, not a replacement for, other medical and lifestyle therapies.
2. How long should I stay in a sauna to target chronic inflammation?
Many experts suggest 10–20 minute sessions, starting shorter and building up, with benefits in studies often seen with multiple weekly sessions at traditional sauna temperatures.
- Acute physiology studies used one or two 10-minute Finnish sauna sessions around 70–90°C (ScienceDirect, 2020).
- Finnish cohorts with health benefits typically used saunas several times per week for 10–20 minutes (PubMed, 2018).
- UCLA recommends starting with 5–10 minutes and limiting total time to 20 minutes (UCLA Health, 2023).
- People with heart disease or high blood pressure are advised to limit sessions to about 10–15 minutes (Healthgrades, 2021).
3. How often should I use a sauna for chronic inflammation relief?
Cohort studies link the greatest benefits with 4–7 sauna sessions per week, but most people start at 2–3 sessions weekly and adjust based on tolerance and medical advice.
- Men using saunas 4–7 times/week had lower hsCRP than those using once/week (PubMed, 2018).
- Frequent sauna bathing was associated with lower cardiovascular and all-cause mortality (PMC, 2022; UCLA Health, 2023).
- Safety guidance emphasizes building up frequency slowly, especially if you have cardiovascular risk (UCLA Health, 2023; Healthgrades, 2021).
4. Is infrared or traditional sauna better for chronic inflammation?
Traditional Finnish saunas have stronger evidence for systemic inflammation and mortality outcomes, while infrared saunas have small trials showing symptom relief in arthritis but limited data on inflammatory markers.
- Finnish cohorts linking sauna to lower hsCRP and mortality involve traditional dry saunas (PubMed, 2018; PMC, 2022).
- Infrared sauna trials in RA and AS show short-term pain and stiffness reductions without worsening disease activity (PubMed, 2009; The Polyclinic, 2022).
- Infrared sauna research provides "limited moderate evidence" for blood pressure improvement (Healthgrades, 2021).
5. Can a sauna help with autoimmune inflammation like rheumatoid arthritis?
Sauna, especially infrared, can help reduce pain and stiffness in RA and similar conditions, but it has not been shown to change disease activity or progression.
- Infrared sauna sessions in RA and AS improved pain and stiffness and reduced fatigue during treatment (PubMed, 2009; University of Twente, 2017).
- No significant changes in RA or AS disease activity scores were observed over 4 weeks (PubMed, 2009).
- Sauna should be used as a complementary therapy alongside disease-modifying medications.
6. Can sauna use make inflammation or pain worse?
Some people, particularly with conditions like ankylosing spondylitis or tendon-dominant disease, report worsened pain or flares with heat, so protocols should be individualized and adjusted if symptoms worsen.
- A user with ankylosing spondylitis reported increased pain and flares with infrared sauna, with a rheumatologist suggesting heat might aggravate tendon involvement (Reddit r/ankylosingspondylitis, 2025).
- Clinical trials in RA/AS did not show disease exacerbation on average, but they were small and short-term (PubMed, 2009).
- It is prudent to reduce time/temperature or stop use if pain consistently worsens.
7. How quickly can sauna use lower CRP or other inflammatory markers?
Single sauna sessions do not lower CRP immediately; lower hsCRP has been observed with frequent use over years, and data on other cytokines are limited and mixed.
- Acute Finnish sauna sessions increased IL-6 and IL-1RA but left CRP unchanged (ScienceDirect, 2020).
- Lower hsCRP in frequent sauna users was observed in long-term cohort follow-up, not acute experiments (PubMed, 2018).
- Heat therapy studies in fibromyalgia showed symptom improvements without significant changes in inflammatory markers (PMC, 2025).
8. What temperature is best for anti-inflammatory sauna benefits?
Traditional saunas in studies are typically 70–100°C, while infrared saunas use lower temperatures; no specific "anti-inflammatory" temperature has been proven, so comfort and safety should guide choice.
- Finnish sauna research generally involves high ambient temperatures characteristic of traditional saunas (PubMed, 2018; ScienceDirect, 2020).
- Infrared saunas operate at lower ambient temperatures while still inducing sweating (PubMed, 2009; Healthgrades, 2021).
- Expert guidance focuses more on session duration and individual tolerance than on a precise degree target (UCLA Health, 2023; Healthgrades, 2021).
9. Is it safe to use a sauna every day for inflammation?
Daily or near-daily sauna use appears safe in healthy adults in Finnish cohorts, but people with heart disease, uncontrolled blood pressure, or other conditions should get medical clearance and may need less frequent sessions.
- Frequent sauna use (4–7 times/week) was associated with lower mortality and hsCRP in Finnish men (PMC, 2022; PubMed, 2018).
- Clinical guidance warns against sauna use in unstable angina, recent MI, severe aortic stenosis, and hypertensive crisis (SIU School of Medicine, 2023; Healthgrades, 2021).
- UCLA recommends conservative session durations and hydration, especially for those with cardiovascular risk (UCLA Health, 2023).
10. Who should avoid using saunas for chronic inflammation?
People with unstable angina, recent heart attack, severe aortic stenosis, hypertensive crisis, or other serious uncontrolled cardiovascular conditions should avoid saunas unless specifically cleared by a physician.
- SIU lists unstable angina, recent MI, and severe aortic stenosis as contraindications (SIU School of Medicine, 2023).
- Healthgrades advises against sauna use when blood pressure is ≥180/110 and stresses caution in those with significant heart disease