What Are the Proven Benefits of Sensory Deprivation Tanks (Float Therapy)?
The Core Benefits at a Glance
Sensory deprivation tanks can deliver strong short-term reductions in stress and anxiety and deep relaxation, but evidence for long-term or disease-specific benefits is mixed.
Key Benefits (What Research Actually Shows):
-
Acute stress and anxiety relief — Large immediate reductions in state anxiety and tension after single 60–90 minute sessions, especially in people with high baseline anxiety (Jonsson et al., 2016; Hope Floats research digest)
-
Deep physical relaxation — Lower blood pressure, slower breathing, and decreased cortisol during and shortly after floats (Khalsa et al., 2022; JEHS review, 2016)
-
Short-term pain and muscle tension reduction — Temporary relief in stress-related pain conditions, though chronic pain benefits don't consistently exceed placebo (Jonsson et al., 2016; JAMA-network RCT, 2021)
-
Mood improvements — Increased serenity, relaxation, and happiness immediately post-float, with reduced depression scores in some trials (Jonsson et al., 2016; feasibility RCT, 2024)
-
Altered states of consciousness — Many users experience boundary dissolution, time distortion, and introspective states that some find therapeutic (Scientific Reports, 2024)
-
Possible sleep support — Subjective reports of better sleep, though systematic reviews find limited evidence for treating formal sleep disorders (BMC systematic review, 2025)
-
Mental clarity and overall well-being — Participants commonly report feeling mentally refreshed and clear-headed for hours to days after sessions (BMC systematic review, 2025)
Critical Caveats:
-
Acute effects are better supported than durable long-term clinical outcomes
-
Most benefits are modest and may require repeated sessions
-
Not all claimed benefits (sleep disorders, athletic performance, magnesium absorption) have strong evidence
-
Should be viewed as an adjunct to, not a replacement for, established medical or psychological treatments
Table of Contents
-
What Sensory Deprivation Tanks Mean
-
Psychological and Mental Health Benefits
-
Physical Health and Athletic Recovery Benefits
-
The Science of REST: How Sensory Deprivation Changes Your Brain
-
Is Float Therapy Right for You? Risks and Contraindications
-
The First-Timer's Guide: What to Expect During Your Float
-
Optimal Floating: Frequency and Duration for Best Results
-
Float Therapy Myths vs. Reality
-
Sensory Deprivation Tanks vs. Other Relaxation Methods
-
Real-World Constraints + Numbers That Matter
-
Experience Layer: Safe Testing Protocol
-
FAQ
-
Sources
-
What We Still Don't Know
What Sensory Deprivation Tanks Mean
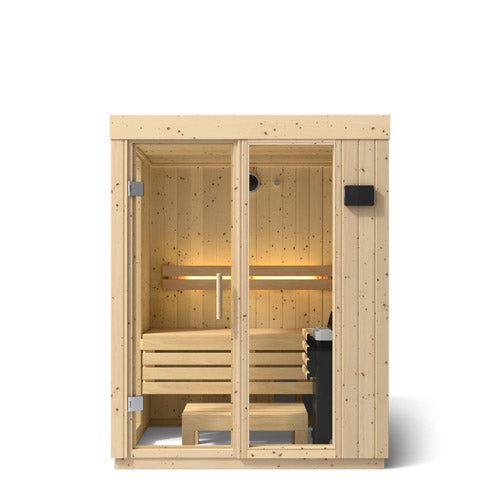
A sensory deprivation tank is a lightless, sound-reduced pod or chamber filled with skin-temperature water saturated with Epsom salt, allowing you to float effortlessly while experiencing minimal external sensory input (Healthline, 2018).
The technical term for float therapy is floatation-REST (Restricted Environmental Stimulation Therapy), a therapeutic technique where individuals float in a dark, quiet, buoyant environment to markedly reduce sensory stimulation and promote deep relaxation (BMC systematic review, 2025).
Key Terms and Mechanisms
REST (Restricted Environmental Stimulation Therapy) refers to controlled procedures that limit sensory input—such as light, sound, and tactile sensations—to study or harness the effects of sensory reduction on physiology and psychology (BMC systematic review, 2025).
How it works:
By dramatically reducing sensory input (sight, sound, touch, proprioception), REST appears to shift the nervous system toward reduced sympathetic arousal and increased parasympathetic activity—essentially moving the body from "fight-or-flight" into "rest-and-digest" mode (Khalsa et al., 2022; Float Hub, 2023).
The water is heated to approximately 93.5°F (34.2°C)—roughly skin temperature—which minimizes thermal sensation. The Epsom salt solution (magnesium sulfate) creates such high buoyancy that floating requires no muscular effort, removing gravitational pressure on joints and allowing the body to achieve a weightless state (Healthline, 2018).
The Autonomic Shift
Parasympathetic dominance describes a nervous system state where "rest-and-digest" activity outweighs "fight-or-flight," often reflected by lower blood pressure, slower heart rate, and increased heart rate variability (HRV) during deep relaxation and float sessions (Khalsa et al., 2022; JEHS review, 2016).
Studies show floatation-REST reduces blood pressure, breathing rate, and certain HRV indices relative to control conditions, suggesting a measurable shift toward parasympathetic dominance (Khalsa et al., 2022).
Understanding sauna and float tank combination therapy can help you leverage both parasympathetic activation and heat-stress benefits for comprehensive recovery.

Psychological and Mental Health Benefits
Acute reductions in state anxiety, tension, and stress after floatation-REST are among the best-supported benefits in the research literature.
Anxiety Relief: The Strongest Evidence
State anxiety—a temporary, situation-dependent form of anxiety reflecting how anxious a person feels at a given moment—drops significantly after single float sessions, particularly in people with high baseline anxiety (Hope Floats research digest; Jonsson et al., 2016).
An open trial in 50 anxious and depressed participants found substantial immediate reductions in state anxiety and improved mood after one 60-minute float, with the largest benefits occurring in those with the highest baseline anxiety scores (Hope Floats research digest).
A 2016 randomized controlled trial (RCT) in stress-related pain conditions showed significant improvements in stress, anxiety, depression, and sleep difficulties after 12 float sessions over 7 weeks, with many outcomes maintained at 6-month follow-up and no serious adverse effects reported (Jonsson et al., 2016).
Short-Term vs. Long-Term Mental Health Effects
What studies actually show:
-
Immediate (minutes to hours): Large drops in state anxiety, muscle tension, and perceived stress; increased feelings of serenity and relaxation (Hope Floats research digest; Jonsson et al., 2016)
-
Short-term (days to weeks): Mood improvements and reduced depression scores, especially in anxious individuals (Jonsson et al., 2016; feasibility RCT, 2024)
-
Long-term (months): Some trials show sustained improvements at 6 months, but large efficacy trials comparing float therapy to gold-standard treatments are still needed (Jonsson et al., 2016; BMC systematic review, 2025)
A 2024 single-blind safety and feasibility RCT in 75 adults with anxiety and depression found that six float sessions were feasible, safe, and well-tolerated, producing positively valenced experiences and few negative effects—but it was not powered for full efficacy outcomes (feasibility RCT, 2024).
Depression Support: An Adjunct, Not a Replacement
Float therapy can temporarily improve mood and reduce depressive symptoms, but it should be viewed as an adjunct to, not a replacement for, standard depression treatments (NCBI evidence brief, 2022; Jonsson et al., 2016).
Studies report mood improvements and reduced depression scores immediately after float sessions, with the largest effects in individuals with comorbid anxiety and depression (Jonsson et al., 2016; Hope Floats research digest). However, evidence for long-term remission or relapse prevention from floating alone is limited (JAMA-network RCT, 2021; NCBI evidence brief, 2022).
Critical caveat: Float therapy is not a replacement for psychotherapy or medication in treating anxiety, depression, or PTSD. Authors and clinicians consistently frame floatation-REST as a complementary tool, and clinical guidelines still prioritize established treatments (Jonsson et al., 2016; feasibility RCT, 2024; NCBI evidence brief, 2022).
Physical Health and Athletic Recovery Benefits
Floatation-REST can acutely decrease perceived pain and muscle tension in some populations, but long-term pain relief beyond placebo is not well supported.
Pain Relief: The Acute vs. Chronic Distinction
Studies in stress-related pain conditions report short-term reductions in pain intensity and muscle tension following multiple float sessions (Jonsson et al., 2016; BMC systematic review, 2025).
However, a rigorous RCT in chronic pain disorder (with psychological and somatic factors) found no clinically meaningful long-term benefit versus an indistinguishable placebo float and wait-list control after five sessions over 3 weeks, with follow-up one week after the last float (JAMA-network RCT, 2021).
Short-term improvements occurred in both the float and placebo groups, demonstrating that placebo and context effects are likely substantial in pain outcomes (JAMA-network RCT, 2021).
Chronic Pain and Fibromyalgia: Why Evidence Is Mixed
The challenge:
-
Most pain trials are small and heterogeneous
-
Protocols vary widely (5–12 sessions, different frequencies)
-
Chronic pain is multifactorial and notoriously difficult to treat
-
Placebo response rates in pain trials are high
A systematic review notes positive effects on pain but stresses the limited number of high-quality RCTs and variability in protocols (BMC systematic review, 2025). An NIH/NCBI evidence brief concludes there is limited evidence overall and insufficient data to recommend for or against tanks for certain physical conditions like symptoms of mild traumatic brain injury (NCBI evidence brief, 2022).
Cardiovascular and Blood Pressure Effects
Studies report reductions in blood pressure, heart rate, and cortisol consistent with deep physical relaxation, which may indirectly support recovery and cardiovascular health (JEHS review, 2016; Khalsa et al., 2022; Hope Floats research digest; BMC systematic review, 2025).
A cardiovascular RCT found that floatation-REST versus a control film condition reduced systolic and diastolic blood pressure, breathing rate, and certain HRV indices, interpreted as a shift to parasympathetic dominance (Khalsa et al., 2022). Diastolic BP decreased roughly twice as much as systolic in some studies, with noticeable changes occurring after 5–15 minutes (JEHS review, 2016).
Important note: Not all studies show significant blood pressure changes, and effects may be transient. People with very low baseline blood pressure should use caution (JEHS review, 2016; Khalsa et al., 2022).
Athletic Performance and Recovery: Limited Evidence
Evidence for improved athletic performance or muscle recovery exists but is limited and often based on small samples; benefits may relate more to relaxation and reduced perceived soreness than objective performance gains (BMC systematic review, 2025; Global Wellness Institute, 2025).
A 2025 systematic review of approximately 63 studies and 1,800 participants found positive effects on athletic performance but emphasized insufficient high-quality data to draw firm conclusions (BMC systematic review, 2025; Global Wellness Institute, 2025).
Magnesium Absorption: The Unsupported Claim
Claims that float tanks significantly correct systemic magnesium deficiency via skin absorption are not well supported (NCBI evidence brief, 2022; Healthline, 2018).
Epsom salt baths are widely claimed to increase magnesium levels, but clinical evidence for substantial transdermal absorption is limited and inconsistent (NCBI evidence brief, 2022). Most float research focuses on psychological and physiologic outcomes, not magnesium kinetics, and marketing often overstates this mechanism (NCBI evidence brief, 2022; Healthline, 2018).
The Science of REST: How Sensory Deprivation Changes Your Brain
Floatation-REST reduces external sensory load, which appears to down-regulate activity in brain networks associated with threat detection and salience while promoting a relaxed, introspective state (Scientific Reports, 2024; Float Hub, 2023; BMC systematic review, 2025).
Altered States of Consciousness
Altered state of consciousness (ASC) is a mental condition in which perceptions of time, body boundaries, and self-awareness shift, as reported by many participants during floatation-REST sessions (Scientific Reports, 2024; Global Wellness Institute, 2025).
A 2024 experimental study comparing floatation-REST versus bed-REST showed significantly more relaxation, less fatigue, and greater anxiety reduction in the float condition, as well as stronger ASC experiences including loss of body boundaries and time distortion (Scientific Reports, 2024; Global Wellness Institute, 2025).
Not everyone experiences vivid ASC phenomena—responses vary widely—but experimental work confirms that float conditions produce measurably stronger perceptual alterations than simple resting environments (Scientific Reports, 2024).
The Ganzfeld Effect and Sensory Deprivation Hallucinations
The Ganzfeld effect occurs when the brain is deprived of structured visual input and begins to fill in the gaps, sometimes producing simple visual or auditory hallucinations similar to those reported in sensory deprivation (Healthline Ganzfeld, 2020; Wikipedia Ganzfeld).
Sensory deprivation hallucinations are perceptual experiences (e.g., flashes of light, shapes, or sounds) that arise when the brain intensifies internal noise due to prolonged lack of external stimuli (Healthline Ganzfeld, 2020; Wikipedia Ganzfeld).
These experiences are typically mild and non-threatening in float settings, though people with certain psychiatric histories might find them distressing and are routinely excluded from research protocols (ClinicalTrials.gov NCT03899090; Scientific Reports, 2024).
Autonomic Nervous System and Parasympathetic Dominance
Autonomic measures demonstrate reduced sympathetic arousal and a shift toward parasympathetic dominance: lower blood pressure, slower breathing, HRV changes, and lower cortisol (Khalsa et al., 2022; Hope Floats research digest; BMC systematic review, 2025; Float Hub, 2023).
A cardiovascular RCT in 37 clinically anxious and 20 non-anxious participants found that float sessions reduced BP, breathing rate, and certain HRV indices relative to a film control; blood pressure reductions correlated with anxiety reduction and increased serenity (Khalsa et al., 2022).
Meta-analytic and review work reports decreased cortisol and stress biomarkers post-float, though methods and sample sizes vary across studies (Hope Floats research digest; BMC systematic review, 2025).
Is Float Therapy Right for You? Risks and Contraindications
Most healthy adults can use commercial float tanks safely, but there are specific contraindications and situations where medical clearance is advised (Blue Lagoon FAQ, 2022; Public Health Ontario, 2016; NCCEH, 2016).
Who Should Avoid or Seek Medical Clearance
People with uncontrolled epilepsy or seizure disorders should avoid floatation tanks without medical clearance due to drowning and fall risk if a seizure occurs in the tank (Blue Lagoon FAQ, 2022; ClinicalTrials.gov NCT03899090; Scientific Reports, 2024).
Individuals with very low blood pressure or fainting risk may experience dizziness or syncope when standing after deep relaxation (Blue Lagoon FAQ, 2022; JEHS review, 2016).
Those with serious cardiac disease, uncontrolled medical conditions, or under active cancer treatment should obtain physician clearance before floating (Blue Lagoon FAQ, 2022; NCBI evidence brief, 2022).
People with open wounds, active skin infections, or recent contagious illnesses are at increased risk of spreading or acquiring infections (Public Health Ontario, 2016; NCCEH, 2016).
First-trimester pregnancy is commonly treated as a precautionary period where float therapy is avoided due to heightened sensitivity and critical fetal development; those with high-risk pregnancies should discuss float therapy with obstetric providers (Floatwell pregnancy guide, 2024; Utah Therapeutic Massage pregnancy guide, 2025).
Individuals with severe claustrophobia or certain psychotic disorders are routinely excluded from research protocols and may not tolerate the enclosed, dark environment (ClinicalTrials.gov NCT03899090; Scientific Reports, 2024).
Known Risks and Adverse Effects
Infection (skin, ear, eye, and genitourinary) is a recognized but preventable risk of float tank use. Public health reviews identify reported infections linked to poorly maintained tanks and highlight vulnerabilities to Pseudomonas, Acanthamoeba, Staphylococcus, and Mycobacterium (NCCEH, 2016; Public Health Ontario, 2016).
Environmental public health guidance states users remain vulnerable to skin, ear, and genitourinary infections and notes possible inhalation exposure risks if water is vigorously agitated (NCCEH, 2016). However, absolute risk appears low where maintenance and disinfection are adequate, and data on infection rates are sparse (Public Health Ontario, 2016; NCCEH, 2016).
Discomfort or stinging from the highly concentrated magnesium sulfate solution can occur on broken skin, cuts, or mucous membranes (NCCEH, 2016).
Anxiety, panic, or exacerbation of claustrophobia in enclosed, dark spaces affects some users, particularly those with pre-existing claustrophobia or certain anxiety disorders (Reddit anxiety discussion; Healthline, 2018).
Slips and falls entering or exiting wet tanks, especially for those with mobility issues, balance problems, or low blood pressure (Blue Lagoon FAQ, 2022; NCCEH, 2016).
Infection Control, Sanitation Standards, and Regulatory Oversight
Float tank infection risk refers to the possibility of users acquiring skin, ear, eye, or genitourinary infections from inadequately disinfected floatation tanks, though such events appear uncommon with proper maintenance (NCCEH, 2016; Public Health Ontario, 2016).
Well-run centers follow strict filtration and disinfection protocols. Guidelines call for regular filtration, chemical disinfection (typically hydrogen peroxide, UV, or ozone), and monitoring of water quality (NCCEH, 2016). The high salt concentration alone is not sufficient for disinfection (NCCEH, 2016).
Reported infections are often linked to inadequate maintenance, disinfection failures, or regulatory gaps (Public Health Ontario, 2016). Customers can and should ask centers about their sanitation procedures, filtration systems, and regulatory compliance.
When to Talk to a Doctor
Before using a float tank if you:
-
Are pregnant or planning to become pregnant
-
Have cardiovascular disease, kidney problems, epilepsy, or severe skin conditions
-
Have complex psychiatric histories or are taking medications that affect blood pressure, balance, or alertness
-
Experience persistent dizziness, severe anxiety, or unusual neurologic symptoms after a float session
The First-Timer's Guide: What to Expect During Your Float
Typical sessions last 45–90 minutes in shallow, highly salted, skin-temperature water, often with pre-float showering and post-float rinsing (Utah Therapeutic Massage cost guide, 2025; Healthline, 2018).
Standard Session Flow
Pre-float (10–15 minutes):
-
Arrive early; many centers recommend arriving 15 minutes before your scheduled time
-
Shower thoroughly to remove oils, lotions, and cosmetics
-
Insert earplugs (provided by facility) to keep salt water out
-
Enter the tank nude (most common) or in a swimsuit
During the float (45–90 minutes):
-
The pod or room will be dark and quiet; some facilities offer optional music for the first and last few minutes
-
Water is shallow (typically 10–12 inches) but the buoyancy is so strong you cannot sink
-
You may drift into the walls initially—this is normal as your body adjusts
-
Many people fall asleep; the salt keeps you afloat even while sleeping (Freeze & Float Spa, 2019; Healthline, 2018)
-
Optional: you can leave the door/lid open or use a dim light if claustrophobia is a concern
Post-float (10–15 minutes):
-
Rinse thoroughly in the shower to remove salt from skin and hair
-
Many facilities provide a relaxation area with tea or water
-
Some people feel slightly disoriented or "floaty" for a few minutes—move slowly and hydrate
What You Might Notice (Non-Guaranteed)
Users may experience a period of adjustment (drifting into walls, difficulty relaxing, mental restlessness) before settling into deeper relaxation (Freeze & Float Spa, 2019; Healthline, 2018).
As the session progresses, you might notice:
-
A gradual release of muscle tension
-
Slowed breathing and heartbeat
-
Loss of awareness of body boundaries or position
-
Time distortion (45 minutes may feel like 15 or like 2 hours)
-
Mild visual phenomena (flashes of color, patterns) with eyes closed
-
Deep introspection or stream-of-consciousness thoughts
-
Drowsiness or actual sleep
None of these are guaranteed, and responses vary widely between individuals and even between sessions for the same person.
Cost and Practical Considerations
In the US, a standard 60-minute float session typically costs about $80–100, with introductory offers often in the $50–70 range and extended 90-minute sessions costing $120–150 (Utah Therapeutic Massage cost guide, 2025).
Some centers offer memberships or multi-session packages (e.g., 5 floats for $350) to reduce per-session cost (Body Therapeutics pricing, 2022; Utah Therapeutic Massage cost guide, 2025).
Exploring floatation therapy tanks for home use involves high upfront capital cost (thousands of dollars) plus ongoing maintenance, but provides unlimited access once installed.
Optimal Floating: Frequency and Duration for Best Results
Research protocols commonly use 45–90-minute sessions, once weekly or multiple times per week, over 5–12 sessions, depending on the condition studied (Jonsson et al., 2016; feasibility RCT, 2024; JAMA-network RCT, 2021).
What Clinical Trials Actually Used
Stress-related pain RCT: 12 sessions over 7 weeks (roughly twice weekly), with significant improvements in stress, anxiety, depression, and sleep difficulties; many outcomes maintained at 6-month follow-up (Jonsson et al., 2016).
Chronic pain RCT: 5 sessions over 3 weeks (roughly twice weekly), with follow-up 1 week after the last float; no long-term benefit versus placebo, suggesting short series may not be sufficient for chronic conditions (JAMA-network RCT, 2021).
Anxiety/depression feasibility trial: 6 sessions (often weekly), showing high adherence (≥80%), good tolerability, and few adverse events; format with flexible duration and frequency was acceptable to participants (feasibility RCT, 2024).
Cardiovascular study: Single 90-minute sessions were sufficient to demonstrate acute physiological changes (blood pressure, breathing rate, HRV) in both anxious and non-anxious participants (Khalsa et al., 2022).
Evidence-Based Frequency Guidance
There is no universally agreed "optimal" schedule; frequency may vary by goal, individual response, and practical constraints (BMC systematic review, 2025; NCBI evidence brief, 2022; BMC systematic review, 2025).
Acute benefits (anxiety, stress reduction) often occur after a single session, but possible cumulative effects are seen with multi-session protocols in some trials (Jonsson et al., 2016; Hope Floats research digest).
For exploration or stress management: Many people start with 1–3 sessions spaced 1–2 weeks apart to assess individual response and duration of relief.
For more intensive goals (e.g., chronic pain, trauma-related anxiety): Research suggests weekly or twice-weekly sessions over 6–12 weeks, though long-term benefits remain uncertain.
Systematic reviews emphasize heterogeneity and insufficient data to derive firm dose-response recommendations (BMC systematic review, 2025; NCBI evidence brief, 2022; BMC systematic review, 2025).
Float Therapy Myths vs. Reality
Myth 1: Float tanks permanently cure anxiety after one session
Correction: Studies show strong immediate reductions in state anxiety, but long-term outcomes and relapse prevention are not well established and likely require repeated sessions and/or other treatments (BMC systematic review, 2025; Hope Floats research digest; Jonsson et al., 2016).
Why it persists: Dramatic short-term relief and testimonials are easily generalized into cure narratives.
Myth 2: Float therapy is a proven long-term treatment for chronic pain
Correction: A rigorous RCT in chronic pain disorder found no long-term advantage of five floatation-REST sessions over placebo and wait-list control (JAMA-network RCT, 2021).
Why it persists: Earlier uncontrolled studies and marketing emphasize short-term pain relief without discussing placebo-controlled results.
Myth 3: Magnesium from Epsom salt in tanks reliably corrects magnesium deficiency
Correction: There is little clinical evidence that transdermal magnesium from Epsom salt baths or float tanks significantly increases systemic magnesium levels (NCBI evidence brief, 2022; Healthline, 2018).
Why it persists: Intuitive appeal of "soaking up minerals" and repetition in spa marketing.
Myth 4: Sensory deprivation tanks are inherently dangerous and cause psychosis
Correction: Clinical trials in carefully screened anxious and depressed patients find floatation-REST to be feasible, well-tolerated, and generally safe, with few adverse events recorded (feasibility RCT, 2024; BMC systematic review, 2025; Jonsson et al., 2016).
Why it persists: Media portrayals of extreme isolation and conflation with uncontrolled deprivation scenarios.
Myth 5: Everyone will hallucinate in a float tank
Correction: While altered perception and ASC are common, not all users experience vivid hallucinations, and responses vary widely (Healthline Ganzfeld, 2020; Wikipedia Ganzfeld; Scientific Reports, 2024).
Why it persists: Anecdotes and sensational accounts are more memorable and widely shared.
Myth 6: Float therapy can replace medication and psychotherapy for depression or PTSD
Correction: Experts position floatation-REST as a complementary tool; no evidence supports replacing established treatments with floating alone for serious psychiatric conditions (NCBI evidence brief, 2022; Hope Floats research digest; Jonsson et al., 2016).
Why it persists: Desire for non-pharmacologic "natural" cures and positive early findings.
Myth 7: Infection cannot happen because salt kills all germs
Correction: Public health reviews document infections associated with float tanks and stress that high salt alone does not prevent microbial contamination without proper disinfection and maintenance (Public Health Ontario, 2016; NCCEH, 2016).
Why it persists: Misunderstanding of how disinfection works and oversimplified marketing claims.
Myth 8: Float therapy is safe for everyone without exceptions
Correction: Contraindications include uncontrolled epilepsy, certain cardiovascular conditions, some skin infections, and early pregnancy; many individuals require medical clearance (Floatwell pregnancy guide, 2024; ClinicalTrials.gov NCT03899090; Blue Lagoon FAQ, 2022).
Why it persists: Oversimplified promotional messaging and lack of standardized screening across centers.
Myth 9: Longer sessions are always better
Correction: Most research uses 45–90-minute sessions, and there is no evidence that much longer sessions produce proportionally greater benefits; risks like dehydration and discomfort may increase (BMC systematic review, 2025; Jonsson et al., 2016; JAMA-network RCT, 2021).
Why it persists: "More is better" heuristic and competitive wellness culture.
Myth 10: There is conclusive proof float therapy improves sleep disorders
Correction: Systematic review notes limited or no effect on formal sleep disorders, although some participants report subjective sleep improvements (Global Wellness Institute, 2025; BMC systematic review, 2025).
Why it persists: Subjective experiences of better sleep are easily generalized into broad claims.
Sensory Deprivation Tanks vs. Other Relaxation Methods
Floatation-REST shares mechanisms with other relaxation tools (parasympathetic activation, reduced muscle tension) but achieves sensory reduction in a unique way (Float Hub, 2023; BMC systematic review, 2025).
Experimental Comparisons
Some experimental comparisons (float vs. bed-REST; float vs. chair-REST) suggest float may confer additional relaxation and anxiety benefits over simple resting environments (Scientific Reports, 2024; feasibility RCT, 2024).
A 2024 study comparing floatation-REST versus bed-REST showed significantly more relaxation, less fatigue, and greater anxiety reduction in the float condition, plus stronger ASC experiences (Global Wellness Institute, 2025; Scientific Reports, 2024).
A feasibility RCT with chair-REST as a comparator shows similar safety and feasibility but was not designed or powered to establish superiority on clinical outcomes (feasibility RCT, 2024).
Float vs. Meditation vs. Sauna: Decision Table
|
Aspect |
Float Therapy (Floatation-REST) |
Mindfulness/Meditation |
Sauna/Heat Therapy |
|
Primary mechanism |
Sensory reduction, buoyancy, decreased sympathetic arousal, potential ASC |
Attention training, cognitive reframing, present-moment awareness |
Heat stress, cardiovascular and thermoregulatory responses |
|
Evidence for acute anxiety/stress reduction |
Strong immediate reductions in state anxiety and stress after single sessions in anxious individuals (Jonsson et al., 2016; Hope Floats) |
Strong evidence for chronic stress and anxiety reduction over weeks–months of practice (NCBI evidence brief, 2022) |
Some evidence for relaxation and perceived stress reduction, though often secondary outcomes (NCBI evidence brief, 2022) |
|
Evidence for chronic pain relief |
Mixed; RCT shows no long-term benefit vs. placebo after 5 sessions (JAMA-network RCT, 2021) |
Moderate for some chronic pain conditions as adjunct therapy (NCBI evidence brief, 2022) |
Moderate for pain and stiffness in certain musculoskeletal conditions (NCBI evidence brief, 2022) |
|
Session length & "dose" |
Typically 60–90 minutes, once weekly or several times over weeks (Jonsson et al., 2016; JAMA-network RCT, 2021) |
Often 10–45 minutes daily or several times per week, ongoing (NCBI evidence brief, 2022) |
Usually 10–20 minutes per session, multiple sessions per week depending on tolerance (NCBI evidence brief, 2022) |
|
Key risks/contraindications |
Infection risk, hypotension, seizures, claustrophobia, pregnancy considerations (NCCEH, 2016; Public Health Ontario, 2016; Blue Lagoon FAQ, 2022) |
Generally low risk; possible distress in trauma histories without guidance (NCBI evidence brief, 2022) |
Heat intolerance, cardiovascular strain, dehydration; cautions in heart disease and pregnancy (NCBI evidence brief, 2022) |
Comparing sauna vs hot tub for stress relief alongside float therapy helps clarify which modality best matches your nervous system needs and wellness goals.
No large head-to-head trials directly compare float therapy against mainstream treatments like CBT, medications, or standard meditation programs for clinical conditions (BMC systematic review, 2025; NCBI evidence brief, 2022). Reviews highlight that REST may be a useful adjunct rather than replacement and that evidence quality is lower than for established therapies (BMC systematic review, 2025; NCBI evidence brief, 2022).
Real-World Constraints + Numbers That Matter
Research Scope
63 studies, approximately 1,800 participants: scope of 2025 systematic review of floatation-REST, reporting positive effects on pain, stress, athletic performance, mental well-being, and clinical anxiety (BMC systematic review, 2025; Global Wellness Institute, 2025).
27 studies, 449 participants: meta-analysis of flotation-REST as a stress-management tool, reporting lower cortisol and blood pressure post-float (Hope Floats research digest).
Session Protocols Used in Research
-
12 sessions over 7 weeks: stress-related pain RCT protocol; significant improvements in stress, anxiety, depression, and sleep difficulties with many maintained at 6 months (Jonsson et al., 2016)
-
5 sessions over 3 weeks: chronic pain RCT protocol; no long-term benefit versus placebo at one-week follow-up (JAMA-network RCT, 2021)
-
6 sessions: anxiety/depression feasibility RCT (pool-REST vs. chair-REST), demonstrating ≥80% adherence with few adverse events and good tolerability (feasibility RCT, 2024)
Clinical Outcomes
37% full remission: proportion of treatment-group participants achieving clinically significant change in primary anxiety outcomes at post-treatment in one RCT (Jonsson et al., 2016).
Blood pressure changes: diastolic BP reducing roughly twice as much as systolic, with noticeable change after 5–15 minutes in some studies (JEHS review, 2016).
Cost Ranges (US Market, 2025)
-
Standard 60-minute session: $80–100
-
Introductory/first-time offers: $50–70
-
Extended 90-minute sessions: $120–150
-
Multi-session packages: often $60–75 per session when buying 5–10 sessions upfront
At-Home vs. Professional: Decision Table
|
Aspect |
At-Home Float Tank |
Professional Float Center |
|
Upfront vs. ongoing cost |
High upfront capital cost (thousands of dollars) plus maintenance supplies (Utah Therapeutic Massage cost guide, 2025; Body Therapeutics, 2022) |
Pay-per-session typically $80–100 for 60 minutes, with packages and discounts (Utah Therapeutic Massage cost guide, 2025) |
|
Water quality & sanitation |
Owner responsible for filtration, disinfection, and monitoring; risk if not done correctly (NCCEH, 2016; Public Health Ontario, 2016) |
Professional centers typically follow local health regulations and industry standards for disinfection and turnover (NCCEH, 2016; Public Health Ontario, 2016) |
|
Convenience & frequency |
Unlimited access at home once installed; flexible session times |
Limited by center hours and travel; may encourage planned routine |
|
Safety oversight |
No on-site staff; higher risk if used by people with medical conditions without supervision |
Staff usually available to assist, monitor first-timers, and handle emergencies (Blue Lagoon FAQ, 2022; feasibility RCT, 2024) |
|
Experience quality |
Customizable but may be constrained by space and noise at home |
Purpose-built soundproof rooms, standardized tanks, and support amenities (Healthline, 2018) |
For those considering ownership, the VMax float pod sensory deprivation tank and DreamPod home float tank represent professionally engineered home options with integrated filtration and sanitation systems.
Experience Layer: Safe Testing Protocol
Tracking Template
Session Log (Copy for Each Float):
|
Field |
Your Entry |
|
Date / Time of float: |
|
|
Session length (minutes): |
|
|
Baseline ratings (0–10): |
|
|
Stress: |
|
|
Anxiety: |
|
|
Mood: |
|
|
Pain: |
|
|
Muscle tension: |
|
|
Immediate post-float ratings (0–10): |
|
|
Stress: |
|
|
Anxiety: |
|
|
Mood: |
|
|
Pain: |
|
|
Muscle tension: |
|
|
Sensations during float: |
|
|
Claustrophobia (yes/no/mild): |
|
|
ASC phenomena (boundary loss, time distortion): |
|
|
Discomfort (describe): |
|
|
Next-day sleep notes: |
|
|
Hours slept: |
|
|
Number of awakenings: |
|
|
Restfulness (0–10): |
|
|
Any adverse effects: |
|
|
Skin irritation (yes/no): |
|
|
Ear issues (yes/no): |
|
|
Dizziness (yes/no): |
Safe Mini-Experiments (Non-Medical)
3-session stress test:
Track mood and stress using 0–10 scales before and after 3 float sessions spaced 1–2 weeks apart; note how long any relief lasts and whether benefits accumulate (Hope Floats research digest; Jonsson et al., 2016).
Athletic recovery comparison:
Compare perceived muscle soreness and recovery after a hard workout with and without a float session within 24 hours; log soreness ratings at 24, 48, and 72 hours (Global Wellness Institute, 2025; BMC systematic review, 2025).
Sleep quality log:
Record sleep quality (time to fall asleep, number of awakenings, restfulness rating) on nights following floats versus your usual routine for 2–3 weeks.
What to Document
-
Pre-session state (stress level, physical tension, mood)
-
In-tank experiences (when you first felt relaxed, any unusual sensations, whether you dozed off)
-
Immediate post-float state (energy, clarity, physical sensations)
-
Duration of effects (when did you return to baseline?)
-
Any adverse effects or discomfort
Understanding whether modalities like float therapy work for you often means comparing them to other evidence-based approaches—learning are saunas good for you can provide useful context for heat-based versus sensory-reduction strategies.
FAQ
1. Are sensory deprivation tanks actually good for you?
Sensory deprivation tanks can be beneficial for many adults, especially for short-term reductions in stress, anxiety, and muscle tension, when used safely in reputable facilities (Jonsson et al., 2016; Healthline, 2018; BMC systematic review, 2025).
-
Studies show strong immediate reductions in state anxiety and stress after floatation-REST sessions (Hope Floats research digest; Jonsson et al., 2016)
-
Users often report improved mood, relaxation, and a sense of well-being (BMC systematic review, 2025; Jonsson et al., 2016)
-
Physiological markers like blood pressure and cortisol often decrease during or after floats (JEHS review, 2016; Khalsa et al., 2022; Hope Floats research digest)
-
Long-term outcomes and benefits for specific medical conditions remain less certain (NCBI evidence brief, 2022; JAMA-network RCT, 2021)
2. What are the main benefits of float therapy?
Main benefits include acute stress and anxiety relief, deep physical relaxation, temporary pain and muscle tension reduction, and subjective improvements in mood and mental clarity (Healthline, 2018; Jonsson et al., 2016; BMC systematic review, 2025).
-
Meta-analyses and reviews report positive effects on stress, anxiety, and mental well-being (Hope Floats research digest; BMC systematic review, 2025)
-
Some trials show short-term pain reduction in stress-related pain and muscle tension (Jonsson et al., 2016; BMC systematic review, 2025)
-
Physiological studies demonstrate lowered blood pressure and slowed breathing (JEHS review, 2016; Khalsa et al., 2022)
-
Evidence for long-term disease-specific benefits is still limited (JAMA-network RCT, 2021; NCBI evidence brief, 2022)
3. Does float therapy help with anxiety?
Float therapy appears particularly promising for short-term relief of anxiety symptoms, especially in people who start with high levels of anxiety (BMC systematic review, 2025; Jonsson et al., 2016; Hope Floats research digest).
-
RCTs and open trials report large immediate drops in state anxiety after single sessions (Jonsson et al., 2016; Hope Floats research digest)
-
Feasibility study in anxious/depressed adults found floatation-REST safe and well-tolerated (feasibility RCT, 2024)
-
Participants often report feeling calmer and more serene for hours to days afterward (Hope Floats research digest; Jonsson et al., 2016)
-
Long-term anxiety management should still include established treatments like CBT or medication when indicated (NCBI evidence brief, 2022)
4. Can float therapy help with depression?
Float therapy can temporarily improve mood and reduce depressive symptoms, but it should be viewed as an adjunct to, not a replacement for, standard depression treatments (NCBI evidence brief, 2022; Jonsson et al., 2016; Hope Floats research digest).
-
Studies report mood improvements and reduced depression scores after float sessions (Jonsson et al., 2016; Hope Floats research digest)
-
A feasibility RCT showed positive experiences and safety in depressed individuals (feasibility RCT, 2024)
-
There is little evidence for long-term remission or relapse prevention from floating alone (JAMA-network RCT, 2021; NCBI evidence brief, 2022)
-
People with depression should discuss float therapy with their mental health providers
5. Does float therapy really reduce pain?
Float therapy can reduce pain and muscle tension in the short term for some people, but robust long-term pain relief, especially for chronic pain, is not well supported (BMC systematic review, 2025; JAMA-network RCT, 2021; Jonsson et al., 2016).
-
Stress-related pain RCTs documented short-term pain reductions after multiple floats (Jonsson et al., 2016)
-
Chronic pain RCT found no long-term benefit over placebo after five sessions (JAMA-network RCT, 2021)
-
Reviews classify the evidence for chronic physical conditions as limited (NCBI evidence brief, 2022; BMC systematic review, 2025)
-
Float therapy may complement, but not replace, established pain management strategies
6. How often should you use a float tank to see benefits?
Many research protocols use weekly sessions over several weeks, and some people notice benefits after a single float, but there is no universally agreed "optimal" frequency (feasibility RCT, 2024; JAMA-network RCT, 2021; Jonsson et al., 2016).
-
Studies have used 5–12 sessions over 3–7 weeks depending on condition (JAMA-network RCT, 2021; Jonsson et al., 2016)
-
Acute anxiety relief often appears after one session (Hope Floats research digest; Jonsson et al., 2016)
-
Systematic reviews highlight insufficient data to define a precise dose-response curve (BMC systematic review, 2025; BMC systematic review, 2025)
-
Practical frequency may depend on goals, cost, and individual response
7. How long does a float therapy session last?
Most commercial and research float therapy sessions last about 60 minutes, with some ranging from 45 to 90 minutes (Healthline, 2018; Jonsson et al., 2016; JAMA-network RCT, 2021).
-
Health resources describe standard 60-minute sessions in sensory deprivation tanks (Healthline, 2018)
-
Clinical trials commonly use 60–90-minute floats (Scientific Reports, 2024; Jonsson et al., 2016)
-
Some centers offer shorter first-time sessions and extended 90-minute floats (Body Therapeutics, 2022; Utah Therapeutic Massage cost guide, 2025)
-
Longer sessions are not proven to be better and may increase discomfort for some users
8. Is it safe to fall asleep in a float tank?
Dozing off in a float tank is common and generally safe in supervised, shallow-water environments, but centers still emphasize screening and safety procedures (Freeze & Float Spa, 2019; feasibility RCT, 2024; Healthline, 2018).
-
Tanks use shallow water with high salt content, making full submersion unlikely (Healthline, 2018)
-
Many users report falling asleep during sessions without incident (Freeze & Float Spa, 2019)
-
Clinical studies report few serious adverse events despite many participants relaxing deeply (feasibility RCT, 2024; Jonsson et al., 2016)
-
People with seizure disorders or certain medical conditions may not be safe to sleep in tanks and should avoid floating without medical clearance (ClinicalTrials.gov NCT03899090; Blue Lagoon FAQ, 2022)
9. Who should not use a sensory deprivation tank?
People with uncontrolled epilepsy, very low blood pressure, active infections or open wounds, certain serious illnesses, and those in early pregnancy should generally avoid float tanks or seek medical clearance first (Floatwell pregnancy guide, 2024; Blue Lagoon FAQ, 2022; NCCEH, 2016).
-
Public health and provider guidance list uncontrolled seizures and significant vertigo as contraindications (Blue Lagoon FAQ, 2022; ClinicalTrials.gov NCT03899090)
-
Infection risk is higher with open wounds or skin infections (NCCEH, 2016; Public Health Ontario, 2016)
-
Many providers advise avoiding floats in the first trimester of pregnancy (Utah Therapeutic Massage pregnancy guide, 2025; Floatwell pregnancy guide, 2024)
-
Individuals with severe claustrophobia or psychotic disorders are often excluded from research (ClinicalTrials.gov NCT03899090; Scientific Reports, 2024)
10. What are the negatives or risks of float therapy?
Main risks include potential infection from poorly maintained tanks, aggravation of claustrophobia or anxiety, and issues related to blood pressure, balance, or pre-existing conditions (Public Health Ontario, 2016; NCCEH, 2016; Healthline, 2018).
-
Documented infections involve skin, ear, eye, and genitourinary sites when disinfection fails (NCCEH, 2016; Public Health Ontario, 2016)
-
Some users may experience heightened anxiety or panic in enclosed, dark spaces (Reddit anxiety discussion; Healthline, 2018)
-
Hypotension or dizziness can be problematic when standing after deep relaxation (JEHS review, 2016; Blue Lagoon FAQ, 2022)
-
Most serious risks are mitigated by proper screening, maintenance, and supervision
11. Is float therapy safe during pregnancy?
Floating may be safe for some pregnant individuals later in pregnancy, but first-trimester use is often discouraged, and pregnant people should always consult their obstetric provider first (Utah Therapeutic Massage pregnancy guide, 2025; Floatwell pregnancy guide, 2024).
-
Facilities commonly advise against float therapy in the first trimester as a precaution (Floatwell pregnancy guide, 2024)
-
Healthcare-oriented guides stress discussing float therapy with an obstetrician (Utah Therapeutic Massage pregnancy guide, 2025)
-
Few research data exist on float use in pregnancy (NCBI evidence brief, 2022)
-
High-risk pregnancies or complications may make floating inadvisable
12. How much does a float therapy session cost in the US?
In the US, a standard 60-minute float session typically costs about $80–100, with introductory offers often in the $50–70 range and extended sessions costing more (Utah Therapeutic Massage cost guide, 2025).
-
60-minute sessions commonly priced at $80–100 in many markets (Utah Therapeutic Massage cost guide, 2025)
-
Introductory or first-time packages often discounted to $50–70 (Utah Therapeutic Massage cost guide, 2025)
-
Extended 90-minute or 2-hour floats can cost $120–150 (Utah Therapeutic Massage cost guide, 2025)
-
Some centers offer memberships or multi-session packages to reduce per-session cost (Body Therapeutics, 2022)
13. Can float therapy improve sleep?
Float therapy may help some people feel more relaxed and sleep better subjectively, but systematic reviews find limited evidence for treating formal sleep disorders (Global Wellness Institute, 2025; BMC systematic review, 2025; Jonsson et al., 2016).
-
RCTs report improvements in sleep difficulties as secondary outcomes (Jonsson et al., 2016)
-
Participants often anecdotally report better sleep after sessions (Hope Floats research digest)
-
Large systematic review found limited or no effect on diagnosed sleep disorders (Global Wellness Institute, 2025; BMC systematic review, 2025)
-
Sleep issues should still be addressed with established medical and behavioral treatments
14. How does float therapy affect blood pressure?
Float therapy often lowers blood pressure during sessions, reflecting deep relaxation, though long-term blood pressure changes are less clear (Khalsa et al., 2022; JEHS review, 2016; Hope Floats research digest).
-
Studies report decreased mean arterial, systolic, and diastolic blood pressure during floats (Khalsa et al., 2022; JEHS review, 2016)
-
Diastolic BP may fall roughly twice as much as systolic in some trials (JEHS review, 2016)
-
BP reductions correlate with decreased anxiety and increased serenity (Khalsa et al., 2022; Hope Floats research digest)
-
People with very low baseline BP should use caution
15. What does float therapy feel like?
Many people describe float therapy as a weightless, deeply relaxing experience with reduced sensory input and sometimes altered perception of time and the body (Freeze & Float Spa, 2019; Scientific Reports, 2024; Healthline, 2018).
-
The water is skin-temperature and highly buoyant, minimizing pressure on joints (Healthline, 2018)
-
Some users experience enhanced introspection or mild altered states of consciousness (Scientific Reports, 2024; Global Wellness Institute, 2025)
-
It can take several minutes to stop drifting and settle into stillness (Freeze & Float Spa, 2019)
-
Reactions vary; some feel calm and refreshed, while others feel restless or anxious initially (Reddit anxiety discussion; Healthline, 2018)
16. Is there scientific evidence behind float therapy, or is it just a fad?
There is a growing body of scientific evidence supporting some benefits of float therapy, especially acute stress and anxiety reduction, but research is still developing and not all claims are supported (BMC systematic review, 2025; BMC systematic review, 2025; NCBI evidence brief, 2022).
-
Systematic reviews and meta-analyses summarize positive effects on stress, anxiety, and well-being (BMC systematic review, 2025; Hope Floats research digest)
-
RCTs have been conducted for stress-related pain, chronic pain, and anxiety/depression (feasibility RCT, 2024; JAMA-network RCT, 2021; Jonsson et al., 2016)
-
Evidence is mixed or limited for chronic pain, sleep disorders, and some physical conditions (JAMA-network RCT, 2021; NCBI evidence brief, 2022)
-
Many studies are small and heterogeneous, so more high-quality research is needed
17. Can float therapy be used at home safely?
Home float tanks can be used safely by some people but require rigorous attention to water quality, sanitation, and screening for medical risks, which professional centers typically manage (Utah Therapeutic Massage cost guide, 2025; Public Health Ontario, 2016; NCCEH, 2016).
-
Owners must maintain filtration, disinfection, and monitoring to prevent infections (Public Health Ontario, 2016; NCCEH, 2016)
-
Home setups lack on-site staff to assist with dizziness, panic, or emergencies (Blue Lagoon FAQ, 2022; feasibility RCT, 2024)
-
Upfront cost and space requirements can be substantial (Body Therapeutics, 2022; Utah Therapeutic Massage cost guide, 2025)
-
Individuals with medical conditions should seek medical advice before using home tanks
18. Are hallucinations in a float tank normal?
Mild visual or auditory phenomena can occur in float tanks due to sensory deprivation, but vivid hallucinations are not universal and can vary widely among individuals (Healthline Ganzfeld, 2020; Wikipedia Ganzfeld; Scientific Reports, 2024).
-
The Ganzfeld effect explains how the brain fills in missing sensory information, sometimes creating simple hallucinations (Healthline Ganzfeld, 2020; Wikipedia Ganzfeld)
-
Experimental float studies document altered states of consciousness, including boundary dissolution and time distortion (Scientific Reports, 2024; Global Wellness Institute, 2025)
-
People with certain psychiatric histories might find these experiences distressing (ClinicalTrials.gov NCT03899090; NCBI evidence brief, 2022)
-
Facilities typically advise users to exit the tank if experiences feel overwhelming
19. How clean are sensory deprivation tanks?
Cleanliness varies by facility, but well-run centers follow strict filtration and disinfection protocols, and public health reviews stress that proper maintenance greatly reduces infection risk (NCCEH, 2016; Public Health Ontario, 2016).
-
Guidelines call for regular filtration, chemical disinfection, and monitoring of water quality (NCCEH, 2016)
-
Reported infections are often linked to inadequate maintenance or regulatory gaps (Public Health Ontario, 2016)
-
The high salt concentration alone is not sufficient for disinfection (NCCEH, 2016)
-
Customers can ask centers about their sanitation procedures and regulatory compliance
20. Is float therapy covered by insurance?
In most cases, float therapy is not covered by standard health insurance and is paid out-of-pocket, though policies vary and some wellness programs may subsidize sessions (Utah Therapeutic Massage cost guide, 2025; NCBI evidence brief, 2022).
-
Evidence briefs note limited economic evaluations and unclear cost-effectiveness (NCBI evidence brief, 2022)
-
Many centers market float therapy as a wellness service rather than a medical treatment (Utah Therapeutic Massage cost guide, 2025)
-
Some health savings or flexible spending accounts may reimburse if prescribed, but this is not standard (NCBI evidence brief, 2022)
-
Users should verify coverage directly with insurers and providers
21. Can float therapy help with PTSD?
Float therapy shows promise as an adjunct for trauma-related anxiety and may help some individuals with PTSD symptoms, but it is not a stand-alone treatment and should be integrated with evidence-based trauma therapies.
-
Some clinicians report anecdotal benefits for PTSD patients, especially for hyper-arousal symptoms (Stella Luna Therapy, 2023)
-
The deep parasympathetic activation and safe, controlled environment may reduce threat-response activation (Float Hub, 2023)
-
No large-scale RCTs specifically target PTSD populations with floatation-REST
-
PTSD treatment should prioritize trauma-focused therapies like EMDR and CPT alongside any complementary approaches
22. What should I bring to my first float session?
Most float centers provide everything you need, but bringing a few personal items can enhance comfort.
-
Most centers provide towels, earplugs, body wash, shampoo, and hair dryers
-
You may want to bring: a brush or comb, contact lens case (remove contacts before floating), personal toiletries if you have sensitive skin
-
Avoid shaving or waxing on the day of your float, as the salt water can sting broken skin
-
Remove makeup, lotions, and oils before your session
23. Can I float if I'm claustrophobic?
Many people with mild claustrophobia successfully use float tanks, especially with accommodations, but severe claustrophobia may make floating uncomfortable or unsuitable.
-
Most modern tanks allow you to keep the door or lid open throughout the session
-
Some facilities offer optional dim lighting inside the tank
-
You can exit the tank at any time if you feel uncomfortable
-
Start with shorter sessions (30–45 minutes) to test your tolerance
-
People with severe claustrophobia are often excluded from research protocols for safety and comfort (ClinicalTrials.gov NCT03899090)
24. Do I need to know how to swim to use a float tank?
No swimming ability is required to use a float tank safely due to the extreme buoyancy created by the Epsom salt solution.
-
The water is only 10–12 inches deep but contains approximately 1,000 pounds of Epsom salt
-
The salt concentration (typically 30–35%) makes sinking essentially impossible
-
You float effortlessly on your back without any effort or swimming motion
-
Many non-swimmers use float tanks without issue
25. Can I float if I dye my hair?
Hair dye stability depends on how recently your hair was colored and the type of dye used.
-
Wait at least 7–10 days after coloring before floating to ensure the dye has fully set
-
Semi-permanent and temporary dyes may still leach color into the tank water even after waiting
-
Permanent dyes that have set for 2+ weeks are generally safe
-
Some centers may ask you to wear a swim cap if your hair color is very fresh or unstable
-
Contact your float center ahead of time if you have concerns about recently dyed hair
Sources
-
Lashgari L, Chen et al. "A systematic review of flotation-restricted environmental stimulation therapy (REST)." BMC Complementary Medicine and Therapies, 2025. Study
-
Semantic Scholar. Entry for the BMC systematic review on flotation-REST. Study
-
Jonsson K et al. "Promising effects of treatment with flotation-REST (restricted environmental stimulation technique) on stress-related muscle pain." BMC Complementary and Alternative Medicine, 2016. Study
-
Fibromyalgia/chronic pain RCT. "Flotation Restricted Environmental Stimulation Therapy for Chronic Pain." JAMA-network style RCT, 2021. Study
-
Khalsa SS et al. "Exploring the acute cardiovascular effects of Floatation-REST." Psychophysiology, 2022. Study
-
Scientific Reports. "Induction of altered states of consciousness during Floatation-REST versus Bed-REST." 2024. Study
-
Feasibility RCT. "A randomized controlled safety and feasibility trial of floatation-REST in anxiety and depression." 2024. Study
-
Hope Floats. Blog summarizing 8 key floatation-REST studies (includes 2004 stress meta-analysis and anxiety/depression trials). Research digest
-
JEHS review. "Beneficial health effects of treatment with flotation-REST on stress-related conditions." PDF review, ~2016. Study/Review
-
NCBI Bookshelf. "Floatation Therapy for Physical Conditions." 2022. Agency-linked evidence review (NIH)
-
Public Health Ontario. "Evidence Brief: Risk of Infection in the Use of Floatation Tanks." June 2016. Agency guidance
-
NCCEH. "Float Tanks: Considerations for Environmental Public Health." 2016. Agency/environmental health guidance
-
Healthline. "Sensory Deprivation Tank: Effects and Health Benefits." 2018. Consumer health resource
-
Healthline. "Ganzfeld Effect: Sensory Deprivation Hallucinations." 2020. Consumer health resource
-
Wikipedia. "Ganzfeld effect." Background reference, originally 2007 with updates. Encyclopedia entry
-
Global Wellness Institute. "Flotation Therapy – Wellness Evidence." 2025. Evidence aggregation
-
Float Hub. "Float Therapy Proven Benefits Science." Blog post, 2023. Provider resource
-
Stella Luna Therapy. "Dr Justin Feinstein and the Benefits of Float Tank Therapy." 2023. Clinician commentary
-
Utah Therapeutic Massage. "Float Therapy During Pregnancy – A Complete Guide." 2025. Clinical/wellness guidance
-
Floatwell. "Floatation Tanks and Pregnancy: Navigating Safety and Comfort." 2024. Clinic guidance
-
**Blue Lag