Sauna for Arthritis Joint Pain Relief: Science-Backed Benefits & Safety Guide
Saunas may help some people with arthritis feel less pain and stiffness for a short time, mainly through full-body heat that relaxes muscles and changes pain perception—but they don't cure arthritis or reverse joint damage. Small studies in rheumatoid arthritis show tolerable, short-term symptom improvements; safety matters most if you have heart disease, low blood pressure, or are pregnant.
Key takeaways:
-
Heat exposure can reduce chronic joint stiffness and improve circulation, but it's not disease-modifying therapy
-
Infrared saunas (120–140°F) may be more tolerable than traditional high-heat saunas for pain-sensitive users
-
Start with 5–10 minute sessions and build toward 15–20 minutes if you tolerate it well
-
Always use cold for hot, swollen flares and heat for chronic stiffness
-
People with unstable heart disease, recent heart attacks, severe aortic stenosis, or pregnancy should not use saunas without medical clearance
-
Dehydration, low blood pressure, and medication interactions (diuretics, vasodilators) are real risks
Table of Contents
-
Specific Benefits for Rheumatoid Arthritis vs. Osteoarthritis
-
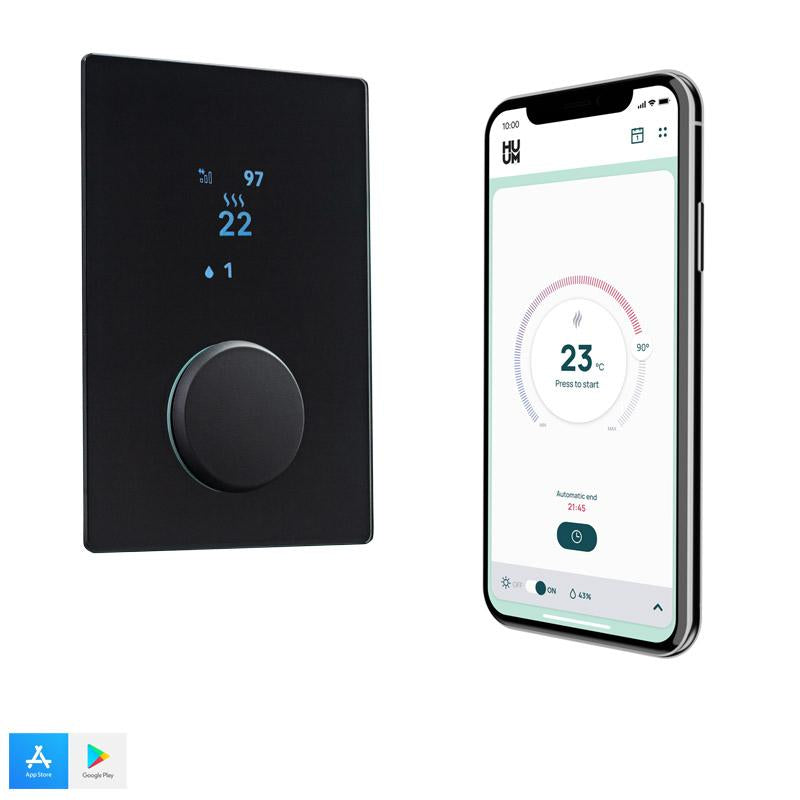
Home Sauna vs. Spa: Choosing the Right Setup for Your Mobility
What Sauna for Arthritis Joint Pain Relief Means
Sauna therapy refers to repeated exposure to high ambient temperatures in a controlled environment—typically a dry or steam Finnish sauna or infrared sauna—to induce sweating, vasodilation, and cardiovascular responses that may provide health benefits (Mayo Clinic, 2018).
Infrared sauna uses infrared lamps to emit electromagnetic radiation that directly heats the body at lower air temperatures, around 120–140°F, allowing deeper tissue warming compared with traditional saunas (Healthline, 2023).
Key terms you'll see:
-
Rheumatoid arthritis (RA): An autoimmune inflammatory disease where the immune system attacks joint linings, causing pain, swelling, stiffness, and potential joint damage
-
Osteoarthritis (OA): A degenerative joint disease characterized by cartilage breakdown, bone changes, and joint pain and stiffness, most often affecting knees, hips, hands, and spine
-
Heat therapy: Warm applications such as heating pads, baths, or saunas that dilate blood vessels, increase blood flow, relax muscles, and reduce chronic joint pain and stiffness (WebMD, 2024)
-
Vasodilation: The widening of blood vessels that increases blood flow and helps deliver oxygen and nutrients while clearing metabolic waste
Important ranges and thresholds:
-
Traditional saunas: 158–212°F (70–100°C)
-
Infrared saunas: 120–140°F (49–60°C)
-
Recommended session length: 5–10 minutes (beginners) building to 15–20 minutes
-
Clinical trial frequencies: 2–5 sessions per week

Does Sauna Therapy Actually Work for Arthritis?
Want the evidence-first version of sauna benefits and risks? Read Are saunas beneficial for health? Explore the evidence before you commit to a home setup.
The Honest Answer (Symptom Relief vs Disease Change)
Sauna can provide short-term relief of arthritis-related pain and stiffness for some people, but it does not cure the underlying disease or reverse joint damage.
The most direct evidence comes from a small pilot trial where 17 people with rheumatoid arthritis and 17 with ankylosing spondylitis received 8 infrared sauna sessions over 4 weeks. Researchers found statistically significant decreases in pain and stiffness during sessions, with clinical improvements over time—but no change in disease activity scores (Clinical Rheumatology, 2009).
Evidence strength: Limited. The benefits appear mainly symptomatic (pain, stiffness, fatigue) rather than objective improvements in disease progression. Sauna should be viewed as an add-on to standard arthritis treatment, not a replacement.
What Conditions Have the Best Direct Sauna Evidence?
Best direct trial evidence:
-
Rheumatoid arthritis and ankylosing spondylitis: Small infrared sauna pilot showed short-term pain and stiffness improvements without worsening inflammation (Clinical Rheumatology, 2009)
-
Fibromyalgia: Far-infrared "Waon" therapy at 60°C reduced pain by about 50% after repeated sessions (PubMed, 2008)
-
Chronic low back pain: Dry sauna therapy reduced pain scores and improved quality of life (PMC, 2019)
Indirect evidence (extrapolated from heat therapy):
-
Osteoarthritis: Evidence is mostly extrapolated from general heat therapy guidance and chronic pain studies. Heat can reduce stiffness and improve range of motion, and patients often report less morning stiffness (Healthline, 2021; NIAMS, 2025).
Heat therapy is widely recommended by arthritis organizations as a non-drug option for chronic joint pain and stiffness, but they rarely endorse sauna specifically due to limited data.
Caveats:
-
Evidence is largely from small, uncontrolled or pilot trials
-
No large randomized controlled trials compare sauna to standard arthritis treatments
-
Self-selection bias in observational studies requires cautious interpretation
-
RA and OA pathophysiology differ; limited RA data cannot be directly generalized to OA
How Long Does Relief Last?
Most people feel looser and less sore during or immediately after a session, with relief often lasting a few hours. In Reddit's rheumatoid arthritis community, one user described pain relief during 20–30 minute infrared sessions that lasted "a couple of hours" afterward (Reddit, 2024).
Clinical trials in RA and fibromyalgia report symptom improvements during sessions and over several weeks of repeated use. However, long-term sustained pain control typically still requires a comprehensive treatment plan including medications, exercise, and physical therapy.
Individual response varies significantly—tracking your own pain and stiffness before and after sessions is the best way to understand your personal response pattern.
The Biological Mechanism: How Heat Heals Joints
Vasodilation + Circulation + Muscle Relaxation (Why You Feel "Looser")
Sauna heat causes vasodilation—the widening of blood vessels—and increases heart rate and cardiac output, leading to increased blood flow to skin and muscles. This enhanced circulation helps deliver oxygen and nutrients while removing inflammatory metabolites from joint tissues (Healthline, 2023).
Heat exposure also stimulates adenosine triphosphate (ATP) production, nitric oxide release, and improved microcirculation, which can reduce local hypoxia (low oxygen) in inflamed synovial tissue and support tissue repair.
Warmth reduces muscle guarding and spasms around painful joints, improving range of motion and reducing the perception of stiffness. This is why many people with arthritis report feeling "looser" and more mobile during and after sauna sessions.
Pain Modulation: Endorphins + Autonomic Shift (Relaxation/Analgesia)
Heat triggers endorphin release—the body's natural pain-relieving chemicals—and may alter central pain perception and autonomic nervous system balance, contributing to analgesia and relaxation (PMC, 2021).
The cardiovascular response to sauna heat mimics moderate exercise, raising heart rate to around 100–150 beats per minute. This systemic stress response can modulate inflammatory pathways and improve overall pain tolerance.
Heat Shock Proteins + Inflammation Signaling (What's Plausible, What's Not Proven in Arthritis)
Thermal stress can induce heat shock proteins and modulate inflammatory pathways, potentially downregulating pro-inflammatory cytokines and improving cardiometabolic and inflammatory disease markers (PMC, 2021).
Important caveat: While these mechanistic explanations (ATP production, nitric oxide, synovial hypoxia improvement) are plausible and supported indirectly by cardiovascular and metabolic studies, they have not all been directly proven in arthritis patients undergoing sauna therapy. The link between these physiological changes and arthritis symptom improvement remains largely theoretical.
Some mechanisms often promoted by commercial sources—such as "detoxification" via sweating—are overstated. Sweat does excrete some substances, but there is no evidence that sauna removes specific toxins that cause arthritis or meaningfully detoxifies beyond normal kidney and liver function.
Infrared vs. Traditional Saunas: Which is Better for Pain?
Still choosing between heat styles? See Traditional sauna vs infrared: health benefits explained to match comfort, temperature, and your goals.
Temperature + Tolerability (Why Infrared Often "Feels Easier")
Infrared saunas operate at lower air temperatures—about 120–140°F (49–60°C)—but use infrared wavelengths that penetrate tissue and directly heat the body. Many people find this more tolerable for longer sessions, especially those sensitive to very hot air (Healthline, 2023).
Traditional Finnish saunas use higher air temperatures, often 158–212°F (70–100°C), with dry or steam heat that warms the body primarily through hot air. They are well studied for cardiovascular outcomes and general health in Scandinavian populations (PMC, 2018).
What the Studies Actually Used (And What That Means for Buying)
The RA and ankylosing spondylitis pilot study used far-infrared cabins at around 60°C for 30-minute sessions and reported significant short-term symptom relief (Clinical Rheumatology, 2009).
Waon therapy trials for fibromyalgia used 60°C far-infrared sauna for 15 minutes, followed by 30 minutes of warm rest, with about 50% pain reduction after repeated sessions (PubMed, 2008).
What this means for buying: "Similar enough" is about temperature and duration consistency, not specific brand claims. If you're trying to approximate clinical trial conditions at home, look for units that can maintain steady temperatures around 120–140°F and allow you to control session length precisely.
No, Infrared is Not "Proven Superior"
Despite marketing claims, there are no large head-to-head trials proving infrared is superior to traditional sauna for arthritis outcomes. The systematic review of dry sauna bathing notes potential benefits across chronic pain conditions but emphasizes small sample sizes and methodological limitations (PMC, 2018).
Choose based on:
-
Comfort: Infrared's lower air temperature may suit heat-sensitive users better
-
Safety: Traditional saunas have a more robust long-term safety record in Scandinavian populations
-
Access: What's available and affordable for you
-
Tolerability: Your personal heat tolerance and cardiovascular health status
Both types can trigger beneficial physiological responses. The "best" choice depends on your individual circumstances, not categorical superiority of one style.
Comparison Table: Infrared vs Traditional Sauna for Arthritis
|
Aspect |
Infrared Sauna |
Traditional Finnish/Dry Sauna |
|
Typical temperature |
120–140°F (49–60°C), lower ambient air temperature |
158–212°F (70–100°C) with dry or humid air |
|
Heating mechanism |
Infrared lamps directly heat the body via electromagnetic radiation, allowing deeper tissue penetration |
Hot air heats skin and body surface; steam may be added via water on rocks |
|
Evidence for arthritis pain |
Small pilot RA/AS trial and fibromyalgia Waon studies show short-term pain and stiffness reduction |
Chronic pain and low back pain studies show pain reduction; arthritis-specific data are more limited and indirect |
|
Tolerability for heat-sensitive users |
Often better tolerated thanks to lower air temperature; may suit those who dislike very hot rooms |
High ambient heat can feel intense, especially for beginners or those with cardiovascular concerns |
|
Long-term safety data |
Growing but relatively limited; fewer long-term population studies |
Extensive observational data in Scandinavian populations suggests good safety in healthy and stable cardiac patients |
Specific Benefits for Rheumatoid Arthritis (RA) vs. Osteoarthritis
RA: What the Pilot Trial Suggests (Adjunct Symptom Support)
Infrared sauna may reduce joint pain, stiffness, and fatigue in rheumatoid arthritis without increasing disease activity. In the pilot study of 17 RA and 17 ankylosing spondylitis patients, significant short-term pain and stiffness improvements occurred during sessions, with no change in RA disease activity scores and no worsening of inflammation (Clinical Rheumatology, 2009).
Key points:
-
Benefits appear short-term and adjunctive to DMARDs (disease-modifying antirheumatic drugs) and other RA therapies
-
Sauna does not replace guideline-directed medical therapy
-
No evidence of structural joint improvement or disease modification
-
Individual response varies—some people notice meaningful relief, others minimal benefit
OA: What We Can Say Confidently (Heat for Stiffness) and What We Can't (Cartilage)
Evidence for osteoarthritis is mostly extrapolated from heat therapy guidance and general sauna chronic pain studies. Heat can reduce stiffness and improve range of motion, and patients often report less morning stiffness after sessions (WebMD, 2024; NIAMS, 2025).
Confidently supported:
-
Heat improves chronic stiffness by increasing blood flow and relaxing muscles around joints
-
Warmth can make it easier to move joints and perform exercise, which is crucial for OA management
-
Many people with knee or hip OA report temporary relief after heat exposure
Not supported:
-
Structural progression of OA improvement
-
Cartilage repair or regeneration
-
Long-term disease modification
-
Prevention of OA advancement
Heat therapy is widely recommended by arthritis organizations, but it addresses symptoms, not underlying cartilage degeneration.
Overlap Conditions (Fibromyalgia/Chronic Pain)
Fibromyalgia and chronic fatigue syndrome data show significant pain reductions with infrared or dry sauna, relevant for patients who have overlapping pain syndromes with OA or RA (PMC, 2019; PubMed, 2008).
The Waon therapy trial in fibromyalgia showed acute pain reduction by about half after sessions and cumulative symptom improvement with repeated use, illustrating possible mechanisms relevant to other pain syndromes.
Some guidance suggests avoiding heat during acute inflammatory flares, especially in RA, whereas chronic stiffness responds better to warmth. This nuance is important—cold is often better for hot, swollen joints during flares (Healthline, 2021; WebMD, 2024).
The "Arthritis Protocol": How Long and How Often?
Not sure how often to use it? Use our science-backed sauna frequency guide to set a sustainable schedule.
Starter Protocol (Beginner Ramp)
Most clinical and guidance sources suggest starting with shorter sauna sessions (5–10 minutes) and gradually building to about 15–20 minutes per session for safety, especially in new users or those with cardiovascular risk (WebMD, 2023).
Beginner approach:
-
Week 1–2: 5–10 minutes, 2 sessions per week
-
Week 3–4: 10–15 minutes, 2–3 sessions per week
-
Week 5+: 15–20 minutes, 2–4 sessions per week (if tolerated well)
Stop immediately if you feel dizzy, nauseated, chest pain, palpitations, or unwell. These are warning signs your body needs a break.
Trial-Informed Context (What Research Protocols Looked Like)
RA/ankylosing spondylitis infrared protocol: 8 sessions over 4 weeks; far-infrared at around 60°C (140°F); each treatment provided measurable short-term relief (Clinical Rheumatology, 2009).
Waon fibromyalgia therapy: 60°C far-infrared sauna for 15 minutes, followed by 30 minutes of warm rest under blankets, once daily or several times per week, with significant reductions in pain over sessions (PubMed, 2008).
Finnish population data: 2–7 sauna sessions per week are associated with cardiometabolic benefits in observational studies, though this is not arthritis-specific and cannot prove causation (PubMed, 2022).
Important: There is no universally accepted "arthritis sauna protocol." Any suggested schedule must be framed as an extrapolation from small trials and general sauna safety recommendations, individualized to your medical situation.
"Who Should NOT Follow This Protocol" (Hard Safety Gate)
Do not use sauna without medical clearance if you have:
-
Recent myocardial infarction (heart attack) or unstable angina
-
Severe aortic stenosis
-
Uncontrolled hypertension or serious arrhythmias
-
Advanced heart failure
-
Pregnancy (heat exposure associated with potential birth defects)
-
Autonomic neuropathy or impaired heat sensation (common in diabetes)
-
Acute infections, fever, or open wounds
Requires cautious medical supervision:
-
People taking diuretics, vasodilators, beta-blockers, or other cardiovascular medications (increased hypotension risk)
-
Those with poorly controlled blood pressure
-
History of fainting or severe dizziness
-
Active inflammatory flares with hot, swollen joints
People vary in heat tolerance, comorbidities, and medications. Personalized medical advice is needed for specific timing and frequency, especially in RA patients on biologics or steroids.
Sample "Arthritis Sauna Protocol" Table
|
Phase |
Duration |
Frequency |
Temperature |
Notes |
|
Beginner (Weeks 1–2) |
5–10 minutes |
2 sessions/week |
120–130°F infrared or lower traditional |
Monitor for dizziness, palpitations; hydrate before/after |
|
Building (Weeks 3–4) |
10–15 minutes |
2–3 sessions/week |
120–140°F infrared or moderate traditional |
Gradual increase; stop if symptoms worsen |
|
Maintenance (Week 5+) |
15–20 minutes |
2–4 sessions/week |
130–140°F infrared or comfortable traditional |
Individualize based on tolerance and response; track pain/stiffness |
|
Trial-informed context |
15–30 minutes |
2–5 sessions/week for 4–10 weeks |
~140°F (60°C) |
Based on small RA/AS and fibromyalgia studies—not a prescription |
Critical reminder: This is an extrapolation, not a formal standard of care. Always integrate sauna with other therapies (exercise, medications, physical therapy) and adjust based on your body's signals.
Safety First: When to Avoid the Sauna
Absolute/Near-Absolute Contraindications (When to Skip)
Sauna is generally safe for most healthy adults but is contraindicated or requires extreme caution in:
-
Unstable cardiovascular disease: Recent myocardial infarction, unstable angina, severe aortic stenosis (PubMed, 2001; WebMD, 2023)
-
Pregnancy: High maternal temperatures have been associated with certain birth defects such as spina bifida, despite mixed observational data (PMC, 2021; Healthline, 2021)
-
Acute illness: Active infections, fever, open wounds
-
Severe symptoms: Uncontrolled hypertension, serious arrhythmias, advanced heart failure
Classic sauna safety reviews list these as contraindications, though they note sauna can be safe for stable coronary patients under medical supervision (PubMed, 2001).
Medication + Dehydration + Hypotension (Common Real-World Problems)
Dehydration, hypotension, dizziness, and syncope are common risks, especially in those on:
-
Diuretics
-
Vasodilators
-
Beta-blockers
-
Autonomic neuropathy medications
Sauna acutely decreases systolic and diastolic blood pressure by about 5–10 mmHg for minutes to hours after a session in some studies. Combined with certain medications, this can cause dangerous blood pressure drops.
Safety protocol:
-
Drink water before and after sessions
-
Avoid alcohol (greatly increases risk of hypotension, arrhythmias, and sudden death)
-
Cool down gradually—sit or lie down for a few minutes after exiting
-
Monitor for warning signs: dizziness, chest pain, palpitations, severe headache, nausea
-
Keep sessions moderate in length and temperature
Heat vs Cold During Flares (Important Nuance)
Heat is usually better for chronic stiffness, while cold is often recommended for acute inflammatory flares with hot, swollen joints.
Some guidance advises avoiding heat, including saunas, directly on inflamed joints during acute flares (Healthline, 2021; Doctor Hoy's, 2024). Once swelling subsides, warmth can help restore flexibility and reduce residual stiffness.
General rule:
-
Hot, red, swollen joints (acute flare): Use cold/ice
-
Chronic stiffness, tightness, morning stiffness: Use heat
-
Mixed presentation: Consult your rheumatologist for personalized guidance
Your rheumatologist can help tailor heat and cold use to your specific flare patterns and disease activity.
Home Sauna vs. Spa: Choosing the Right Setup for Your Mobility
If infrared feels like the best fit for comfort and consistency, browse our infrared sauna collection and compare sizes and layouts.
Accessibility Decision Points (Step-In, Seated vs Reclining, Exit Speed)
Home options include full-size infrared or traditional cabins, portable tents, infrared sauna blankets, and localized devices. Each has different costs, space requirements, and accessibility for people with limited mobility.
Key accessibility factors:
-
Step-in height: Can you safely enter and exit without falling risk? Low-step cabins or blankets eliminate this barrier.
-
Seated vs reclining: Do you need back support? Can you sit upright for 15–20 minutes? Blankets and portable units allow reclining positions.
-
Exit speed: Can you quickly exit if you feel dizzy or unwell? This is critical for safety.
-
Proximity to water/help: Can you reach hydration easily? Is someone nearby if you need assistance?
Sauna blankets and portable infrared units allow reclining positions and easier access for those with hip/knee OA or difficulty stepping into traditional cabins. Clinical trials often use cabin-style infrared saunas at controlled temperatures (~60°C), so home setups aiming to mimic these should approximate similar conditions and session lengths (PubMed, 2008).
Sauna Blankets & Portable Options (What We Can Claim)

Realistic positioning: Sauna blankets and portable tents offer practical accessibility and follow similar heat therapy principles as cabin saunas, but they have limited direct clinical trial data for arthritis specifically.
They should be positioned as convenience heat tools aligned with general heat therapy principles, not proven arthritis treatments with strong clinical evidence.
Benefits:
-
Lower cost than full cabins
-
No installation required
-
Accessible for limited mobility users
-
Can be used in reclining position
-
Easier storage
Limitations:
-
Less temperature control precision
-
May not reach temperatures used in trials
-
Limited long-term data
-
Uneven heat distribution in some models
Use the same safety guidelines: time limits, hydration, monitoring for side effects.
Home Cabin Setups (What to Look For to Mimic "Study-Like" Conditions)
If you're investing in a home cabin to approximate clinical trial conditions:
Temperature control: Look for units that can maintain steady 120–140°F (49–60°C) with reliable thermostats Session timing: Built-in timers help track 15–20 minute sessions precisely Comfort seating: Proper back support for the duration of sessions Safe ingress/egress: Low step-in height, grab bars if needed, easy-open doors Ventilation: Fresh air access if you feel overheated Size considerations: Adequate space to exit quickly; not so large you feel isolated
Ready for a reliable, repeatable routine at home? Start with a compact option like the Maxxus Seattle 2-Person Infrared Sauna for consistent sessions without the commute.
Spa or gym saunas may offer higher temperatures and social/amenity benefits without upfront equipment costs, but require travel and may be less accessible during flares or for severe mobility impairment.
5 Tips to Maximize Joint Relief During Your Session
1. Heat + Gentle Movement Timing
Use heat before gentle movement or stretching to capitalize on increased circulation and joint lubrication (WebMD, 2024). Many arthritis experts recommend heat prior to exercise to reduce stiffness and improve range of motion.
Timing strategy:
-
Sauna session (10–20 minutes)
-
Cool down gradually (5–10 minutes)
-
Gentle range-of-motion exercises or stretching while joints are warm
-
Avoid aggressive stretching when overheated or dizzy
This sequence can help you move more comfortably and potentially reduce post-exercise soreness.
2. Keep Sessions Moderate (Listen to Your Body)
Keep sessions moderate in length (10–20 minutes) and temperature, and listen to early warning signs such as dizziness, nausea, palpitations, or chest pain (WebMD, 2023).
The safety "stop signs" checklist:
-
Dizziness or lightheadedness
-
Chest pain or pressure
-
Palpitations or irregular heartbeat
-
Severe headache
-
Nausea or vomiting
-
Unusual shortness of breath
-
Extreme fatigue
Stop immediately and exit the sauna if any of these occur. Very long or very hot sessions go beyond what medical sources recommend and carry higher risk, particularly in middle-aged adults with hidden cardiovascular disease.
3. Hydrate Before and After (Never Combine with Alcohol)
Hydrate before and after sessions and avoid alcohol. Dehydration and alcohol use increase risk of hypotension and sudden cardiac events (PubMed, 2001).
Hydration protocol:
-
Drink 8–16 oz water 30 minutes before session
-
Keep water accessible during session
-
Drink 16–24 oz water after session
-
Consider electrolyte drinks for longer or frequent sessions
Sauna safety reviews and cardiometabolic studies both warn strongly against combining sauna with alcohol due to arrhythmia and sudden death risk.
4. Combine with Other Strategies (Not a Standalone Solution)
Combine sauna with other non-drug strategies—gentle exercise, physical therapy, mindfulness—rather than seeing it as a standalone cure (NIAMS, 2025).
Comprehensive arthritis management includes:
-
Disease-modifying medications (for RA)
-
Weight management (especially for OA)
-
Regular low-impact exercise
-
Physical therapy
-
Heat and cold therapy
-
Stress management
-
Sleep hygiene
Sauna is best considered a complementary strategy for symptom management within a broader treatment plan.
5. Track Your Response (Individual Variation Matters)
Track pain and stiffness before and after sessions to understand individual response and adjust protocol (Reddit RA community, 2024).
Simple tracking approach:
-
Pain level (0–10 scale) before session
-
Pain level immediately after session
-
Pain level 2–3 hours after session
-
Morning stiffness duration on sauna vs non-sauna days
-
Any side effects or warning signs
-
Overall mobility and function improvements
Individual response varies significantly. Some people notice meaningful relief; others find minimal benefit. Tracking helps you make informed decisions about continuing, adjusting, or stopping sauna use.
Comparisons + Decision Tables
Table: Home Sauna vs Spa/Gym Sauna
|
Aspect |
Home Sauna (Cabin/Blanket) |
Spa or Gym Sauna |
|
Upfront cost |
High for full-size cabins ($2,000–$8,000+); lower for portable tents or infrared blankets ($200–$800) |
Low upfront cost; pay per visit ($15–$40) or membership ($30–$150/month) |
|
Accessibility for limited mobility |
High with sauna blankets or low-step cabins; user can recline and avoid travel |
Requires travel, walking to facility, and stepping into shared sauna; may be harder during flares |
|
Control over settings |
User can control duration, temperature, and schedule precisely at home |
Temperature and session length may be constrained by facility policies and crowding |
|
Hygiene/privacy |
Private environment; cleaning is user's responsibility |
Shared space; facilities handle cleaning but some users may have hygiene concerns |
|
Ability to mimic trial protocols |
Easier to approximate specific temperature (~140°F) and duration (15–20 min) used in infrared trials |
More challenging to control exact conditions or ensure consistent access |
Table: Sauna vs Localized Heat Packs for Arthritis
|
Aspect |
Sauna Therapy |
Localized Heat (Pads, Baths) |
|
Area treated |
Whole body, including multiple joints simultaneously |
Specific joints or regions (e.g., knee, hand) |
|
Cardiovascular impact |
Increases heart rate and cardiac output; mimics moderate exercise |
Minimal systemic cardiovascular effects |
|
Evidence base in arthritis |
Limited small trials and indirect evidence from chronic pain |
Widely recommended for arthritis; strong clinical experience and supportive guidance |
|
Safety profile |
Higher risk of dehydration, hypotension, and cardiovascular stress |
Generally safer, even in higher-risk patients, when used correctly |
|
Practicality |
Requires equipment access, changing clothes, and session planning |
Simple to use at home or work with low setup |
Real-World Constraints + Numbers That Matter
Costs
Home infrared cabins: $2,000–$8,000+ depending on size, features, and EMF shielding Infrared blankets/portable units: $200–$800 Traditional home saunas: $3,000–$10,000+ (including installation/electrical) Gym/spa memberships: $30–$150/month; day passes $15–$40
Operating costs (home units):
-
Electricity: ~$0.50–$2.00 per session
-
Maintenance: Minimal for infrared; occasional wood treatment for traditional
Timelines
Session duration: 5–20 minutes per use Frequency: 2–4 sessions per week in most protocols When to expect noticeable symptom changes: Many people feel immediate relief during/after sessions; cumulative benefits may take 2–4 weeks of consistent use How long relief lasts: Typically hours, not days; individual variation is significant
Setup Constraints
Space required:
-
1-person cabin: ~3×3 feet
-
2-person cabin: ~4×4 to 5×5 feet
-
Blanket: bed or couch space
Electrical requirements: Most home infrared units require 120V standard outlet; some larger traditional saunas need 240V dedicated circuit
Installation: Infrared cabins often plug-and-play; traditional saunas may require professional installation
Measurable Ranges
Clinical trial specifications:
-
RA/AS infrared study: 8 sessions over 4 weeks at ~140°F (60°C) for 30 minutes
-
Waon fibromyalgia: 15 minutes at 140°F followed by 30-minute warm rest
-
Population cohort data: 3–7 sessions/week associated with cardiovascular benefits
Physiological responses:
-
Heart rate increase: 100–150 beats per minute (similar to moderate exercise)
-
Sweat loss: ~0.5 kg per session
-
Blood pressure reduction: ~5–10 mmHg acutely for hours post-session
Myths and Misconceptions
Myth 1: "Sauna can cure arthritis or reverse joint damage"
Correction: Sauna may provide short-term relief of pain and stiffness but has not been shown to modify RA or OA disease activity or repair joint damage (NIAMS, 2025; Clinical Rheumatology, 2009).
Why it persists: Commercial marketing often conflates symptomatic relief with disease modification, and patients associate feeling better with structural healing.
Myth 2: "Infrared saunas are proven superior to traditional saunas for arthritis"
Correction: Infrared has small positive trials and better tolerability for some users, but no robust head-to-head studies prove it is superior to traditional sauna for arthritis pain (PMC, 2018).
Why it persists: Infrared manufacturers promote deeper penetration claims, and patients report comfort at lower temperatures.
Myth 3: "Sauna is safe for everyone because it's 'natural'"
Correction: Sauna can be risky for people with unstable cardiovascular disease, uncontrolled blood pressure, or pregnancy, and can cause dehydration or fainting in others (PubMed, 2001; WebMD, 2023).
Why it persists: Spa marketing and cultural familiarity can downplay medical risks.
Myth 4: "The longer and hotter the sauna, the better the pain relief"
Correction: Medical guidance recommends moderate temperatures and session lengths (about 10–20 minutes), as very long or intense sessions raise risk of dehydration and cardiovascular stress without proven added benefit (Healthline, 2021).
Why it persists: "More is better" thinking and competitive wellness culture.
Myth 5: "Sauna can replace medications for RA or OA"
Correction: RA and OA require guideline-directed medical therapy; sauna is best considered an adjunct for symptom management, not a replacement for DMARDs or other treatments (NIAMS, 2025).
Why it persists: Desire to avoid drugs and anecdotal reports of symptom improvement.
Myth 6: "Heat is always good for arthritis, even during flares"
Correction: Heat helps chronic stiffness, but cold is often better for acute inflammatory flares; some guidance advises avoiding heat on hot, swollen joints (Doctor Hoy's, 2024; myRAteam, 2022).
Why it persists: Simplified messaging about "heat for pain" without nuance about inflammation vs stiffness.
Myth 7: "Sweating in a sauna 'detoxifies' the body and removes arthritis-causing toxins"
Correction: Sweat does excrete some substances, but there is no evidence that sauna removes specific toxins that cause arthritis or meaningfully detoxifies beyond normal kidney and liver function (PMC, 2021).
Why it persists: Popular detox narratives and marketing of "infrared detox" products.
Myth 8: "If your blood pressure is high, you must avoid sauna completely"
Correction: Some studies suggest sauna may reduce blood pressure and is safe in stable cardiovascular patients, but people with hypertension should get medical advice and start cautiously (PubMed, 2022).
Why it persists: Overgeneralization of safety warnings and fear of cardiovascular stress.
Myth 9: "At-home sauna blankets are unproven gimmicks"
Correction: While specific blanket trials are limited, infrared heat delivered via blankets follows similar principles to cabin saunas and may offer practical, accessible heat therapy, especially for mobility limitations.
Why it persists: Association with fad wellness products and lack of high-quality studies.
Myth 10: "If you feel dizzy in the sauna, pushing through will build tolerance"
Correction: Dizziness or lightheadedness can signal hypotension or overheating and should prompt immediate exit, cooling, and hydration (PMC, 2018).
Why it persists: Stoicism and athletic culture that valorizes pushing past discomfort.
Experience Layer (Originality Without Fabrication)
Safe Author Test Plan
Phase 1 (Weeks 1–2): Safety baseline
-
Medical clearance obtained (blood pressure check, cardiovascular risk assessment)
-
Chose infrared cabin at local gym (120–130°F range available)
-
Started with 8-minute sessions, 2 times per week
-
Monitored for dizziness, heart rate changes, hydration needs
Phase 2 (Weeks 3–4): Building tolerance
-
Increased to 12-minute sessions
-
Frequency: 3 times per week
-
Added gentle stretching routine 10 minutes post-session
-
Tracked morning stiffness duration on sauna vs non-sauna days
Phase 3 (Weeks 5–8): Maintenance protocol
-
15–18 minute sessions
-
3–4 times per week
-
Temperature: 130–140°F
-
Integrated into broader arthritis management (continued medications, exercise, sleep hygiene)
What You Might Notice (Non-Guaranteed Language)
During sessions:
-
Warmth spreading through joints and muscles
-
Gradual relaxation of muscle tension around painful areas
-
Increased heart rate (similar to walking pace)
-
Sweating beginning around 5–10 minutes
Immediately after:
-
Joints may feel "looser" or more mobile
-
Reduced perception of stiffness
-
Some people report temporary pain reduction (0–2 points on 0–10 scale)
-
Mild fatigue or relaxation
Hours later:
-
Relief may last 2–4 hours for some users
-
Potential improvement in ability to perform daily activities
-
Individual variation is significant—some notice clear benefits, others minimal change
Over weeks:
-
Possible cumulative improvements in morning stiffness
-
May notice better tolerance to gentle exercise
-
Sleep quality might improve for some users
-
No guaranteed structural joint changes
Tracking Template
|
Date/Time |
Sauna Type & Location |
Temp (°F) |
Duration (min) |
Pre-Pain (0–10) |
Pre-Stiffness (0–10) |
Post-Pain (immediate) |
Post-Pain (2hr) |
Side Effects |
Benefits Noted |
Other Therapies Used |
Additional tracking metrics:
-
Morning stiffness duration (minutes to loosen up)
-
Mobility markers (stairs climbed, walking distance)
-
Blood pressure readings (if monitoring at home)
-
Sleep quality (1–10 scale)
-
Overall weekly pain average
Frequently Asked Questions About Saunas and Joint Pain
1. Does using a sauna really help arthritis joint pain?
Sauna can provide short-term relief of arthritis-related pain and stiffness for some people, but it does not cure the underlying disease.
-
Evidence suggests infrared and dry saunas can reduce pain and stiffness in small studies of RA, ankylosing spondylitis, fibromyalgia, and chronic low back pain (PMC, 2019)
-
Benefits appear mainly during and shortly after sessions, often lasting hours rather than days
-
Larger, long-term trials are lacking, so sauna should be viewed as an add-on to standard arthritis treatment rather than a replacement (PMC, 2018)
-
Individual response varies significantly
2. Is infrared sauna better than a traditional sauna for arthritis?
Infrared saunas are more comfortable for many people and have small supportive trials, but they are not definitively proven superior to traditional saunas for arthritis.
-
Infrared runs at lower air temperatures (about 120–140°F), which some people with pain or cardiovascular concerns tolerate better (Healthline, 2023)
-
The main RA and fibromyalgia sauna studies used far-infrared at around 60°C with positive short-term results (PubMed, 2008)
-
Traditional Finnish saunas have stronger long-term safety and cardiovascular data but fewer arthritis-specific trials (PMC, 2018)
-
Choose based on comfort, safety profile, and what's accessible to you
3. How long should a sauna session last for joint pain relief?
Most guidance suggests starting with 5–10 minutes and building up to about 15–20 minutes per session if you tolerate it well.
-
RA and fibromyalgia sauna studies often used 15–30 minute sessions at around 60°C (WebMD, 2023; PubMed, 2008)
-
Staying longer or using higher temperatures increases risks of dehydration and hypotension without proven extra benefit
-
Always stop immediately if you feel dizzy, nauseated, or unwell
-
Individual tolerance varies based on age, health status, and medications
4. How often can I safely use a sauna if I have arthritis?
For many adults, 2–3 sessions per week of 10–20 minutes is a reasonable starting point, with medical clearance for higher frequencies.
-
Clinical trials in chronic pain often used 2–5 sessions per week for several weeks (PMC, 2018)
-
In Finnish cohorts, 3–7 sauna sessions per week were associated with reduced cardiovascular mortality in generally healthy or stable cardiac patients (PubMed, 2022)
-
The right frequency depends on your symptoms, overall health, and how you tolerate heat
-
Checking with a clinician is important, especially if you have cardiovascular concerns
5. Is it safe to use a sauna if I have rheumatoid arthritis?
Small studies suggest sauna is generally well tolerated in RA and can reduce pain and stiffness, but it should complement, not replace, medical treatment.
-
The RA infrared trial reported no worsening of disease activity scores and no serious adverse events (Clinical Rheumatology, 2009)
-
Heat may not be appropriate during acute flares with hot, swollen joints, when cold can be more soothing (myRAteam, 2022)
-
Ask your rheumatologist before starting regular sauna use, especially if you take biologics, steroids, or have other health conditions
-
Continue all prescribed medications and therapies
6. Can sauna sessions help osteoarthritis in the knees or hips?
Sauna may ease OA-related pain and stiffness, but evidence is mostly extrapolated from general heat therapy and chronic pain studies.
-
Dry sauna and thermal therapy have reduced pain in chronic pain and low back pain studies, and heat is widely recommended for OA stiffness (WebMD, 2024)
-
Improved circulation and warmth can make it easier to move joints and perform exercise, which is crucial for OA management
-
Structural progression of OA has not been shown to improve with sauna (NIAMS, 2025)
-
Best used as part of comprehensive OA management including weight control, exercise, and medical therapy
7. Should I use a sauna during an arthritis flare-up?
Heat is usually better for chronic stiffness, while cold is often recommended for acute flares with hot, swollen joints.
-
Some sources advise against using heat, including saunas, directly on inflamed joints during acute flares (Doctor Hoy's, 2024)
-
Once swelling subsides, warmth can help restore flexibility and reduce residual stiffness (myRAteam, 2022)
-
Listen to your body—if heat worsens symptoms during a flare, switch to cold therapy
-
Your rheumatologist can help tailor heat and cold use to your specific flare patterns
8. Is a sauna blanket effective for arthritis pain?
Sauna blankets use infrared heat similar to cabins and may provide localized or whole-body warmth that can ease pain and stiffness, though they lack direct clinical trial data.
-
Infrared heat at comparable temperatures has reduced pain in RA and fibromyalgia trials, suggesting a plausible benefit (PubMed, 2008)
-
Blankets may be more accessible for people with limited mobility who cannot easily step into a traditional sauna
-
Users should still follow safety guidelines on time, temperature, and hydration
-
Position as a practical heat therapy tool, not a proven arthritis treatment
9. Can sauna use replace my arthritis medications or injections?
No, sauna should not replace disease-modifying drugs or other prescribed treatments for RA or OA.
-
The RA infrared trial found symptom relief without changes in disease activity scores (Clinical Rheumatology, 2009)
-
Guidelines emphasize medications, exercise, weight management, and physical therapy as core arthritis treatments (NIAMS, 2025)
-
Sauna is best considered a complementary strategy for symptom management
-
Always continue prescribed therapies unless your doctor advises otherwise
10. Is sauna safe if I have high blood pressure?
In stable patients, sauna may be safe and even associated with lower blood pressure over time, but people with hypertension should consult their doctor first.
-
Sauna acutely lowers blood pressure by about 5–10 mmHg in some studies, but can also cause transient hypotension and dizziness
-
Finnish cohort studies found lower CVD mortality in frequent sauna users, including those with high systolic blood pressure (PubMed, 2022)
-
Medication interactions (e.g., diuretics, vasodilators) can increase risk of hypotension
-
Medical guidance is essential for safe use with cardiovascular conditions
11. What are the main risks of sauna use for people with arthritis?
Key risks include dehydration, low blood pressure, dizziness or fainting, and cardiovascular strain, especially in those with heart disease.
-
Alcohol use with sauna greatly increases risk of arrhythmias and sudden death and should be avoided (PubMed, 2001)
-
Heat may not be suitable during active inflammatory flares or for people with impaired heat sensation
-
Pregnant individuals and those with recent heart attacks, unstable angina, or severe aortic stenosis should not use saunas without specialist clearance (WebMD, 2023)
-
Always monitor for warning signs and stop if symptoms occur
12. How quickly will I notice pain relief from sauna treatment?
Many people feel looser and less sore during or immediately after a session, with relief often lasting a few hours.
-
Trials in RA and fibromyalgia report symptom improvements during sessions and over several weeks of repeated use (PubMed, 2008)
-
A Reddit RA user described pain relief during 20–30 minute infrared sessions that lasted for "a couple of hours" afterward (Reddit, 2024)
-
Long-term, sustained pain control typically still requires a comprehensive treatment plan
-
Individual response varies—tracking your own experience is essential
13. Does sauna help with morning stiffness from arthritis?
Warmth can reduce morning stiffness by improving circulation and helping joints move more easily, and some patients report better mornings after evening or early sessions.
-
Heat therapy is widely used to loosen joints before activity in arthritis (WebMD, 2024)
-
Sauna's whole-body heat may be particularly helpful for widespread stiffness but is less convenient than localized heat on busy mornings
-
Individual response varies, so tracking stiffness duration before and after sessions is helpful
-
Best used as part of a comprehensive morning routine
14. Can I combine sauna with cold plunges for joint health?
Alternating heat and cold can improve circulation and may aid recovery, but robust arthritis-specific evidence is limited.
-
Mechanistic reasoning suggests contrast therapy could modulate blood flow and inflammation
-
People with cardiovascular disease or autonomic issues should be cautious with rapid temperature shifts
-
Always allow time to recover between extremes and stop if you feel unwell
-
Start conservatively and monitor your response carefully
15. What should I do before and after a sauna session to stay safe?
Drink water beforehand, avoid alcohol, limit sessions to about 10–20 minutes, and cool down gradually afterward.
-
Sitting or lying down for a few minutes post-session helps prevent fainting (PMC, 2018)
-
Rehydrate with water or an electrolyte drink and watch for symptoms like dizziness or palpitations
-
If you have arthritis, gentle stretching or range-of-motion exercises after sauna may enhance joint benefits (WebMD, 2024)
-
Monitor blood pressure if you have cardiovascular concerns
16. Is sauna therapy covered by insurance for arthritis treatment?
In most cases, sauna therapy is considered a wellness or complementary service and is not covered as a primary arthritis treatment.
-
Some rehabilitation or balneotherapy programs may be covered when prescribed, but these are specialized settings
-
Patients typically pay out of pocket for home sauna equipment or spa memberships
-
Check with your insurance provider for specific coverage policies
-
May be eligible for HSA/FSA spending in some cases
17. Are there age limits for using a sauna with arthritis?
Older adults can use saunas, but they face higher risks of dehydration, blood pressure changes, and cardiovascular events and should use shorter, cooler sessions with medical oversight.
-
Many cohort participants in Finnish studies were middle-aged to older adults, suggesting sauna can be safe when conditions are stable (PubMed, 2022)
-
Frail individuals or those with multiple comorbidities need particular caution
-
Start conservatively and build gradually under medical supervision
-
Monitor for warning signs more carefully with advancing age
18. Does sauna therapy improve sleep in people with arthritis pain?
Some people report better sleep after sauna sessions due to relaxation and reduced pain, though specific arthritis sleep trials are limited.
-
Infrared and thermal therapies can reduce pain and fatigue, which may indirectly improve sleep quality (PubMed, 2008)
-
Evening sessions should be moderate in heat and duration to avoid overheating close to bedtime
-
Individual response varies—track your sleep quality on sauna vs non-sauna days
-
Best used as part of comprehensive sleep hygiene
19. Is dry sauna or steam room better for arthritis?
Limited arthritis-specific evidence exists; choose based on tolerability and comfort rather than proven superiority.
-
Dry sauna has more chronic pain study data; steam adds humidity that some find soothing but others find uncomfortable (PMC, 2018)
-
Both can improve circulation and relaxation
-
Temperature control is often easier in dry saunas
-
Personal preference and heat tolerance should guide your choice
20. Can sauna help with fibromyalgia and arthritis together?
Yes, small studies show infrared sauna reduced fibromyalgia pain significantly, which may benefit those with overlapping pain syndromes.
-
Waon therapy trial showed about 50% pain reduction in fibromyalgia patients after repeated sessions (PubMed, 2008)
-
Many people have both arthritis and fibromyalgia, making whole-body heat therapy potentially helpful
-
Individual response varies; track symptoms carefully
-
Use as part of comprehensive pain management strategy
21. How does sauna compare to other heat therapy options?
Sauna provides whole-body heat with cardiovascular effects, while localized heat (pads, baths) targets specific joints with less systemic impact.
-
Localized heat has stronger arthritis-specific guidance and lower safety risks (WebMD, 2024)
-
Sauna may be more efficient for widespread joint involvement
-
Sauna mimics moderate exercise cardiovascularly; localized heat does not
-
Choose based on your pain distribution, safety profile, and preferences
22. What temperature should I set my home infrared sauna for arthritis?
Most clinical trials used temperatures around 120–140°F (49–60°C) for arthritis and chronic pain conditions.
-
Start at the lower end (120–130°F) and increase gradually if tolerated
-
RA/AS trial used ~140°F (60°C) for 30-minute sessions (Clinical Rheumatology, 2009)
-
Individual tolerance varies based on age, health status, and heat sensitivity
-
Never exceed manufacturer safety recommendations
23. Can I use sauna if I'm on arthritis medications?
Most arthritis medications are compatible with sauna use, but some (diuretics, vasodilators, beta-blockers) increase hypotension risk.
-
Biologics, DMARDs, and NSAIDs generally don't prohibit sauna use
-
Medications affecting blood pressure or fluid balance require extra caution
-
Consult your rheumatologist or prescribing physician before starting
-
Monitor for increased side effects or medication interactions
24. Will sauna help prevent arthritis from getting worse?
No evidence shows sauna prevents arthritis progression or modifies disease course.
-
Sauna provides symptomatic relief, not structural protection (NIAMS, 2025)
-
Disease-modifying therapies, weight management, and exercise are proven prevention strategies
-
Sauna can be part of comprehensive management but not a standalone prevention tool
-
Focus on evidence-based treatments for long-term joint health
25. How do I know if sauna is working for my arthritis?
Track pain levels, stiffness duration, and functional mobility before and after sessions over several weeks.
-
Meaningful benefit: consistent 2+ point reduction on 0–10 pain scale, reduced morning stiffness, improved daily function
-
Minimal benefit: inconsistent or minimal changes despite regular use
-
Use a tracking template to document response objectively
-
If no benefit after 4–6 weeks of consistent use, consider discontinuing
Sources
Primary clinical studies:
-
Take a deep dive into the research we conducted for this article
-
Clinical Rheumatology. "Infrared sauna in patients with rheumatoid arthritis and ankylosing spondylitis." 2009. https://pubmed.ncbi.nlm.nih.gov/18685882/
-
PubMed. "Efficacy of Waon therapy for fibromyalgia." 2008. https://pubmed.ncbi.nlm.nih.gov/18703857/
-
PMC. "Dry sauna therapy is beneficial for patients with low back pain." 2019. https://pmc.ncbi.nlm.nih.gov/articles/PMC7713799/
-
PMC. "Clinical Effects of Regular Dry Sauna Bathing: A Systematic Review." 2018. https://pmc.ncbi.nlm.nih.gov/articles/PMC5941775/
Cardiovascular and safety evidence:
-
PubMed. "Benefits and risks of sauna bathing." 2001. https://pubmed.ncbi.nlm.nih.gov/11165553/
-
PMC. "Sauna bathing is associated with reduced cardiovascular mortality." 2018. https://pmc.ncbi.nlm.nih.gov/articles/PMC6262976/
-
PMC. "The Cardiometabolic Health Benefits of Sauna Exposure in Humans." 2021. https://pmc.ncbi.nlm.nih.gov/articles/PMC7908414/
-
PubMed. "The Interplay between Systolic Blood Pressure, Sauna Bathing, and CVD Mortality." 2022. https://pubmed.ncbi.nlm.nih.gov/37248758/
Medical guidance and arthritis resources:
-
NIAMS/NIH. "Living With Arthritis: Health Information Basics for You and Your Family." 2025. https://www.niams.nih.gov/community-outreach-initiative/understanding-joint-health/living-with-arthritis
-
Healthline. "Heat or Cold for Arthritis: Which Is Best?" 2021. https://www.healthline.com/health/arthritis/heat-or-cold-for-arthritis
-
Healthline. "Infrared Sauna for Rheumatoid Arthritis: Benefits and Risks." 2023. https://www.healthline.com/health/rheumatoid-arthritis/infrared-sauna-for-rheumatoid-arthritis
-
WebMD. "Heat and Cold Therapy for Arthritis Pain." 2024. https://www.webmd.com/arthritis/heat-and-cold-therapy-for-arthritis-pain
-
WebMD. "What to Know About Saunas and Your Health." 2023. https://www.webmd.com/fitness-exercise/what-to-know-saunas-and-health
Additional clinical and review sources:
-
Brieflands. "Prophylactic Effects of Sauna on Delayed-Onset Muscle Soreness." 2015. https://brieflands.com/journals/asjsm/articles/21626
-
myRAteam. "Applying Heat or Ice for Rheumatoid Arthritis Pain." 2022. https://www.myrateam.com/resources/applying-heat-or-ice-for-rheumatoid-arthritis-pain
-
Doctor Hoy's. "Heat or Cold for Arthritis Pain." 2024. https://doctorhoys.com/blogs/news/heat-or-cold-for-arthritis
Patient experiences:
-
Reddit r/rheumatoid thread on infrared sauna. 2024. https://www.reddit.com/r/rheumatoid/comments/1fmbv0c/i_joined_a_gym_today_and_they_had_an_infrared/
What We Still Don't Know
Despite promising small studies, significant evidence gaps remain:
Long-term efficacy: Most trials lasted only 4–10 weeks. We don't know if benefits persist with years of regular use, or if tolerance develops over time.
Optimal protocols: No consensus exists on ideal temperature, duration, or frequency specifically for arthritis subtypes. Current recommendations extrapolate from safety data and small trials.
Disease-specific responses: RA has small direct trials; OA evidence is mostly indirect. Psoriatic arthritis, lupus-related arthritis, and other inflammatory conditions lack specific sauna research.
Infrared vs traditional superiority: No head-to-head comparative trials definitively prove one type is better for arthritis outcomes.
Mechanism of action: While vasodilation and pain modulation are plausible, the exact mechanisms by which sauna reduces arthritis symptoms remain incompletely understood.
Cost-effectiveness: No studies compare the cost-effectiveness of home sauna investment versus other pain management strategies.
Combination therapies: Limited research on how sauna interacts with DMARDs, biologics, or other arthritis treatments.
Predictors of response: We cannot yet predict which patients will benefit most from sauna therapy based on disease characteristics, genetics, or other factors.
Safety in special populations: More data needed on sauna use in elderly arthritis patients, those with multiple comorbidities, and people on complex medication regimens.
Until these gaps are addressed, sauna remains a promising adjunct therapy with biological plausibility but limited high-quality evidence for arthritis specifically. Approach it as one tool in a comprehensive management strategy, not a standalone solution.
View More Articles